Simultaneous-to-Implant placement GBR
Dr. David González
DDS, M.Sc, PhD Master in Periodontics EFP and PhD Doctor at Complutense University of Madrid.
Private practice at Clínica Ortoperio in Murcia, Spain.
Facts
Patient:
28 years old woman, ex-smoker, medically healthy.
Clinical problem:
Patient presented a hopeless 21 (actually the tooth was loose, attached by composite to the adjacent teeth) and although being spaniard caucasian she had a severe melanosis and gummy smile.
Clinical solution:
To treat a severe bone dehiscence in the esthetic zone, simultaneous implant placement with guided bone regeneration (GBR) was performed using a titanium-reinforced NeoGen® PTFE membrane, 100% autogenous bone, and a Neoss ProAcitve® implant.
Treatment plan:
- Extraction of 21. Socket preservation using Xenograft (anorganic bovine hydroxylapatite-collagen), non cross-link collagen membrane and connective tissue graft.
- 9 months later: after seeing by a CBCT that no bone augmentation was gained a Simultaneous-to-implant placement GBR procedure to regenerate a severe bone dehiscence.
- 100% autogenous bone was used as a filling material. It was evident that due to the CTG from the palate (where there was no melanosis) the appearance of the gingiva was less pigmented.
- 9 months later: Reentry was carried out, removing the membrane, connecting an 8 mm healing abutment and placing a “poncho” connective tissue graft from the palate.
- 3 months later: A screw-retained zirconia-porcelane crown was delivered and a general peeling at both upper and lower gingiva was carried out.
Products:
1 NeoGen® Ti-Reinforced PTFE Membrane.
1 Neoss ProActive® Implant 4.5 mm x 13 mm
Conclusion:
After 5 years of implant-supported screw-retained crown delivery hard and soft tissue stability was observed and an esthetic appearance was achieved.
Simultaneous-to-Implant placement GBR using a PTFE, Ti-reinforced NeoGen® membrane and 100% autogenous bone is a fully predictable treatment for the severe bone dehiscenceon the Aesthetic Zone. This statement is supported clinical exam and periapical x-ray.
Step by step
Step by step
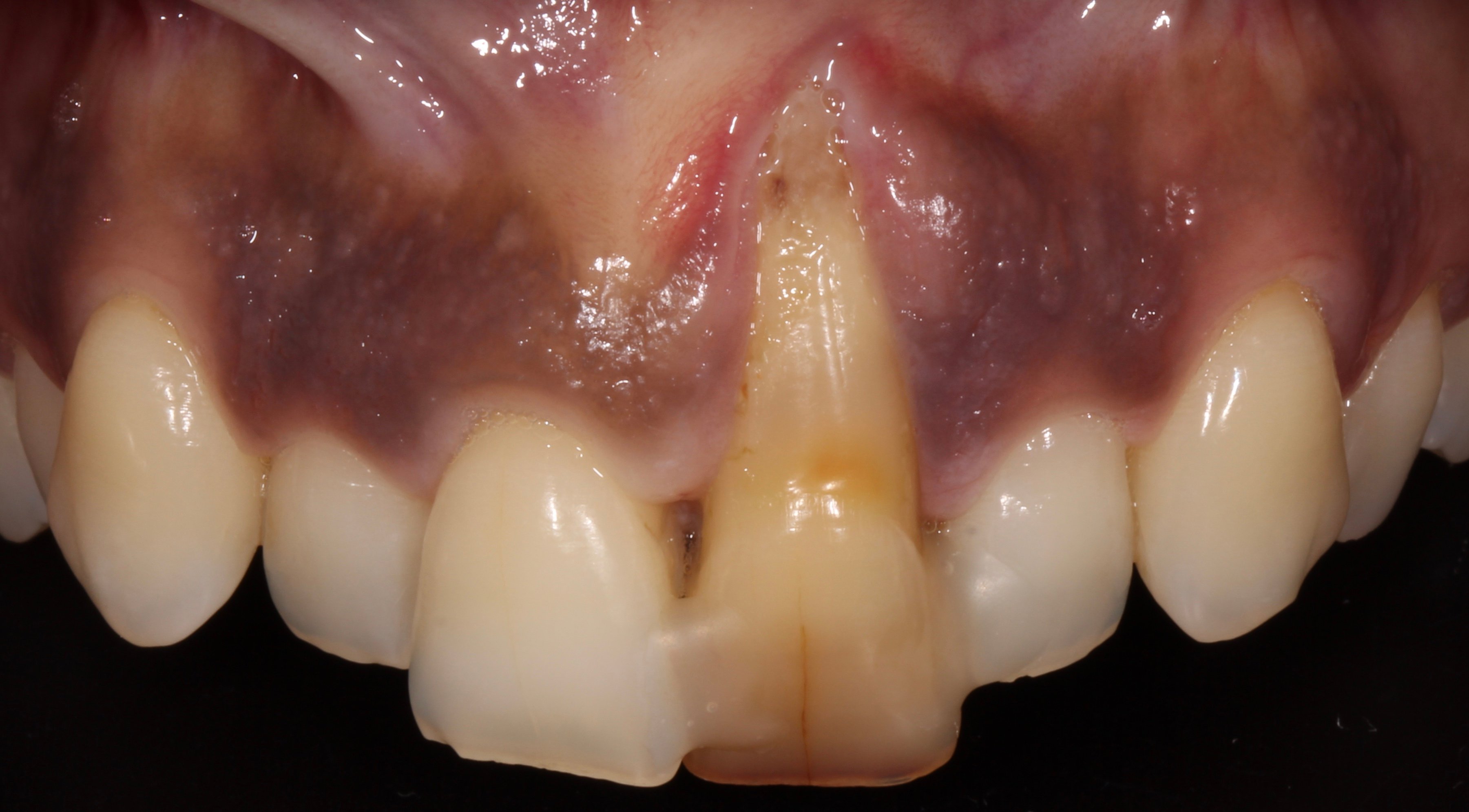
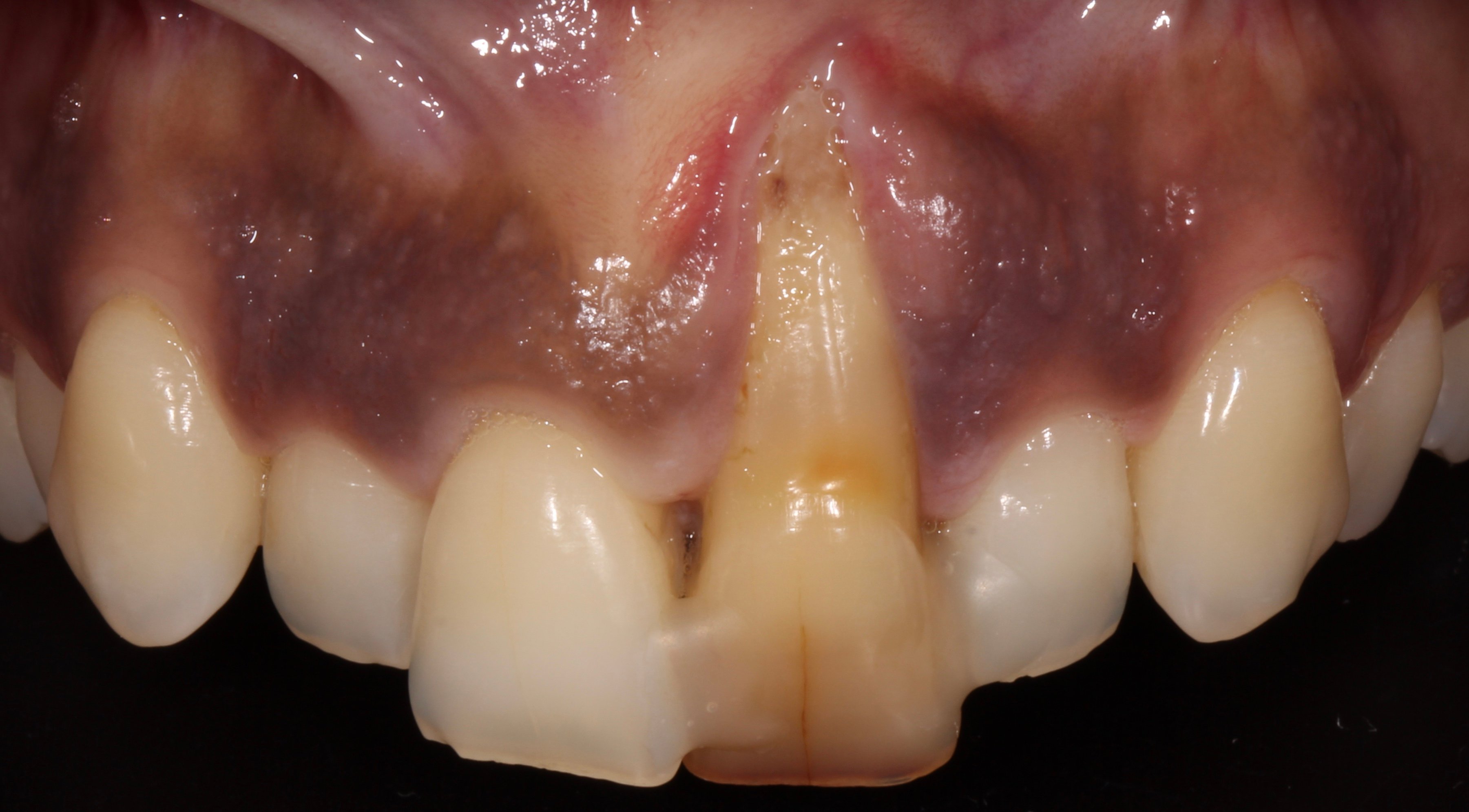
Figure 1.

Figure 2.
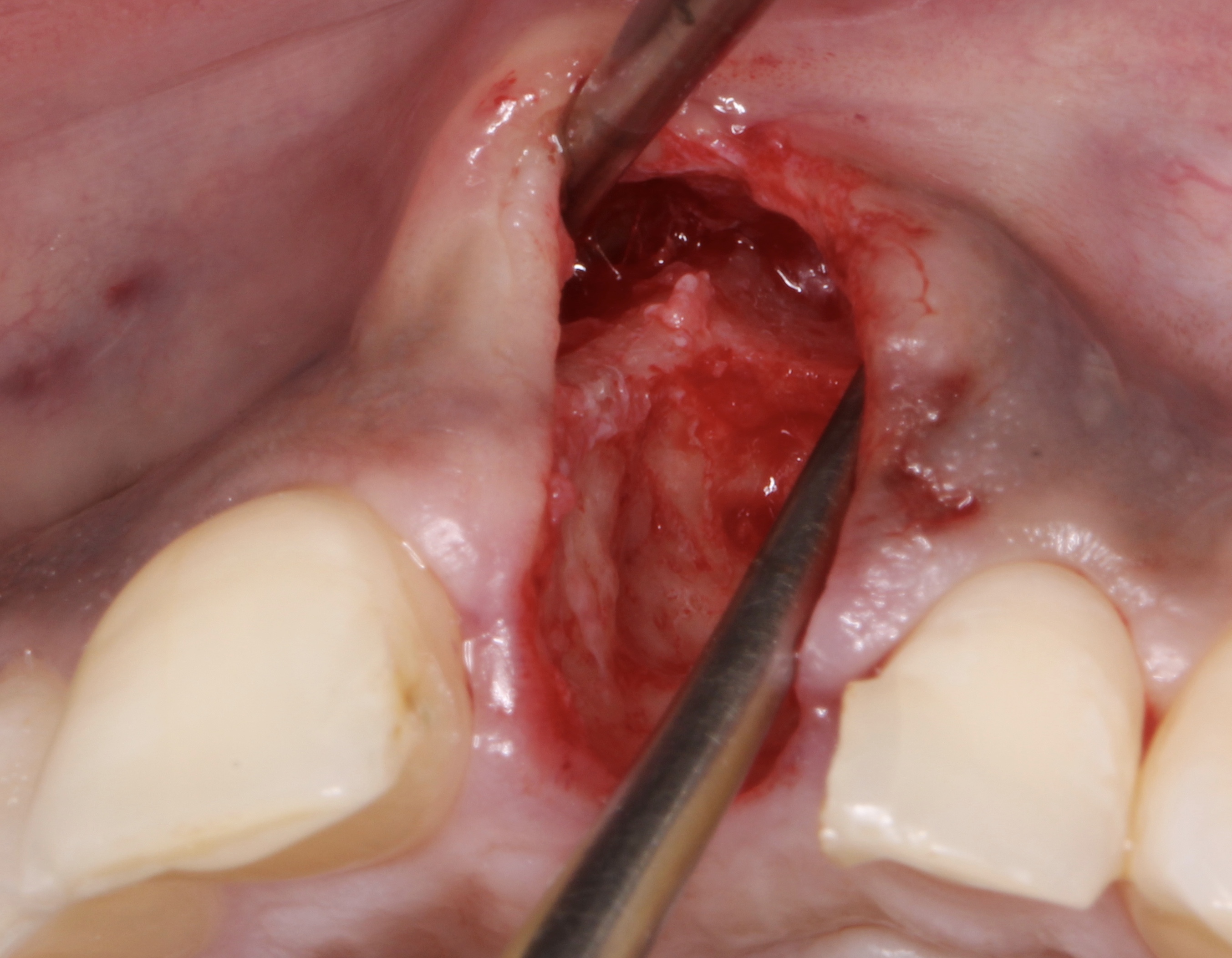
Figure 3.
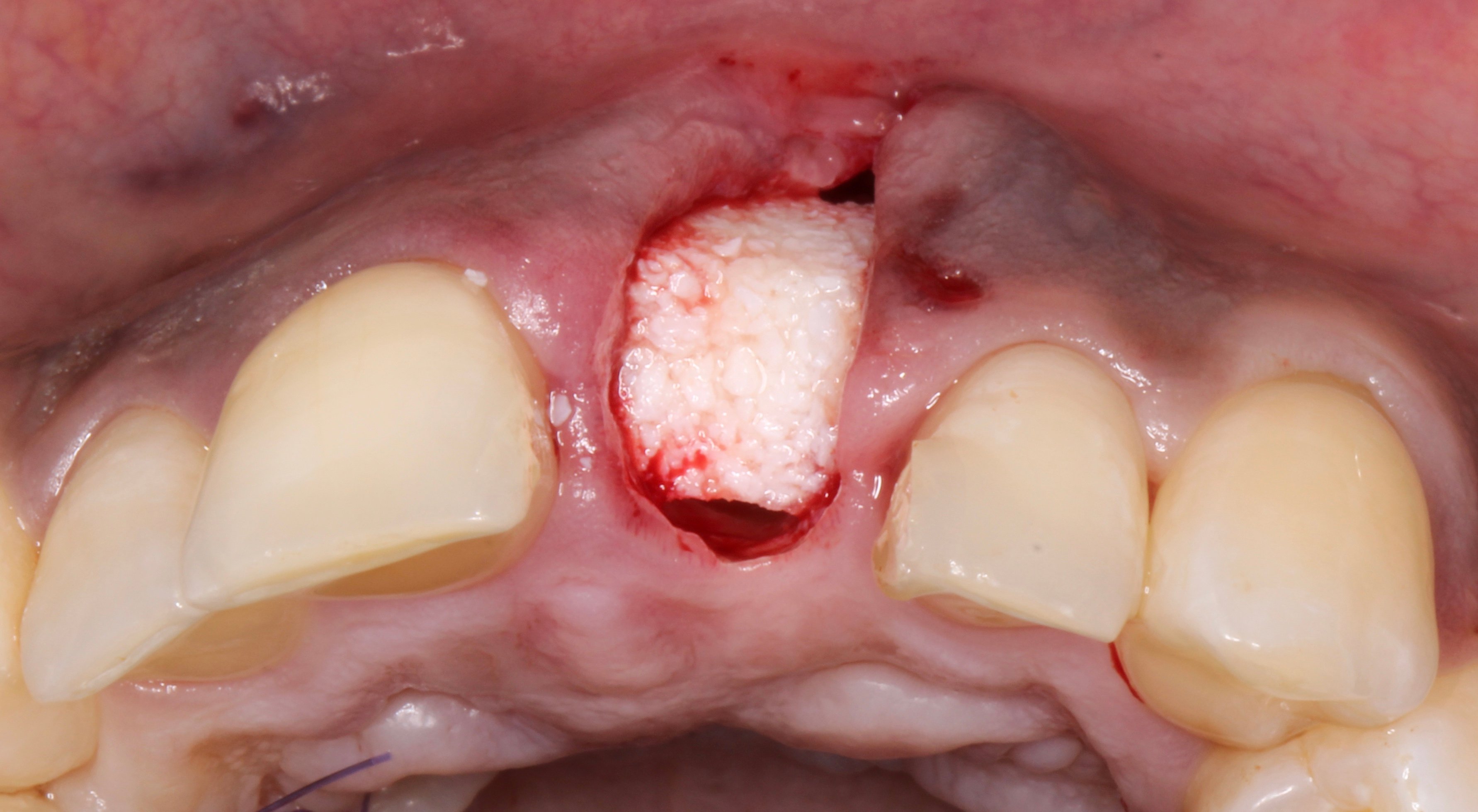
Figure 4.
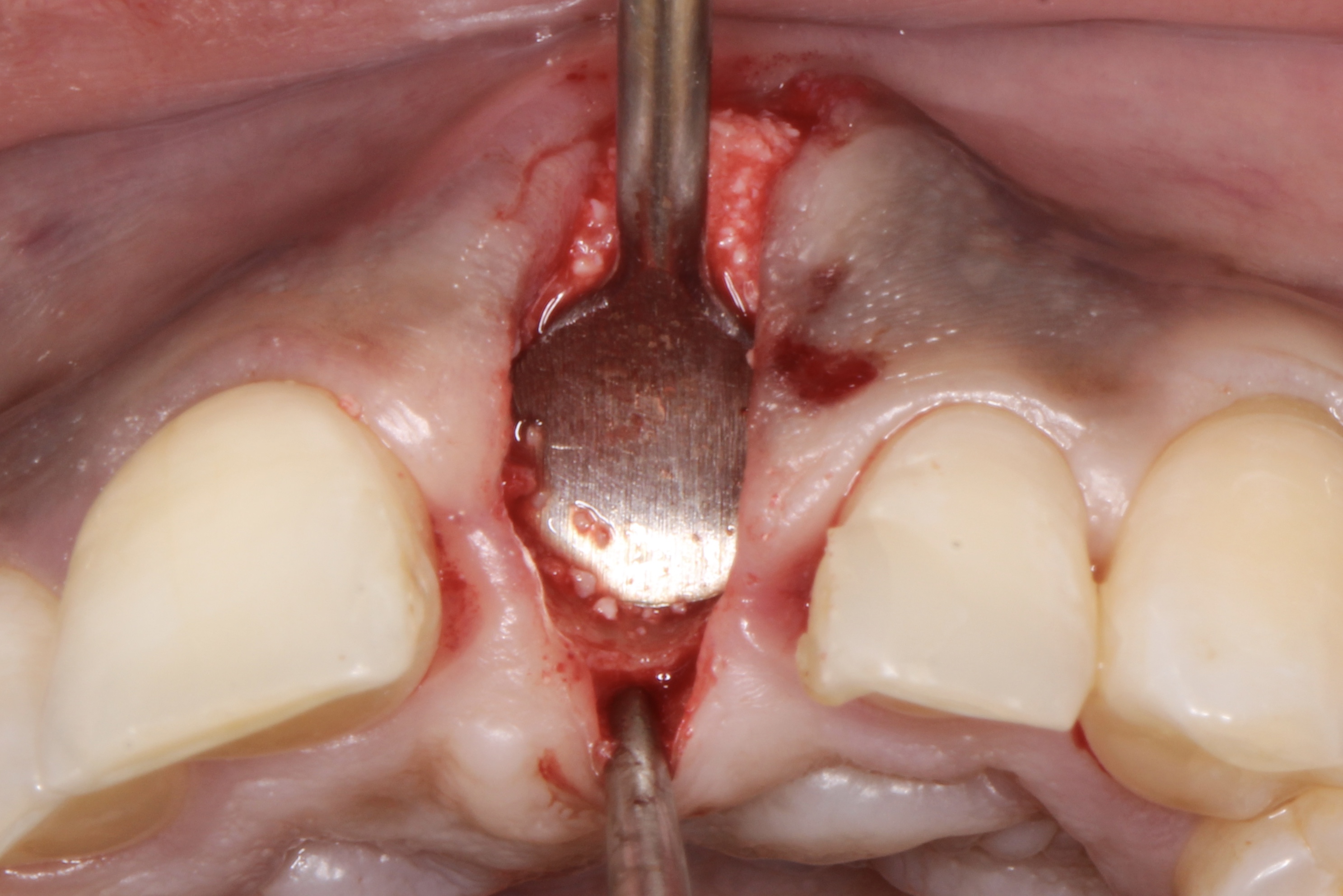
Figure 5.

Figure 6.
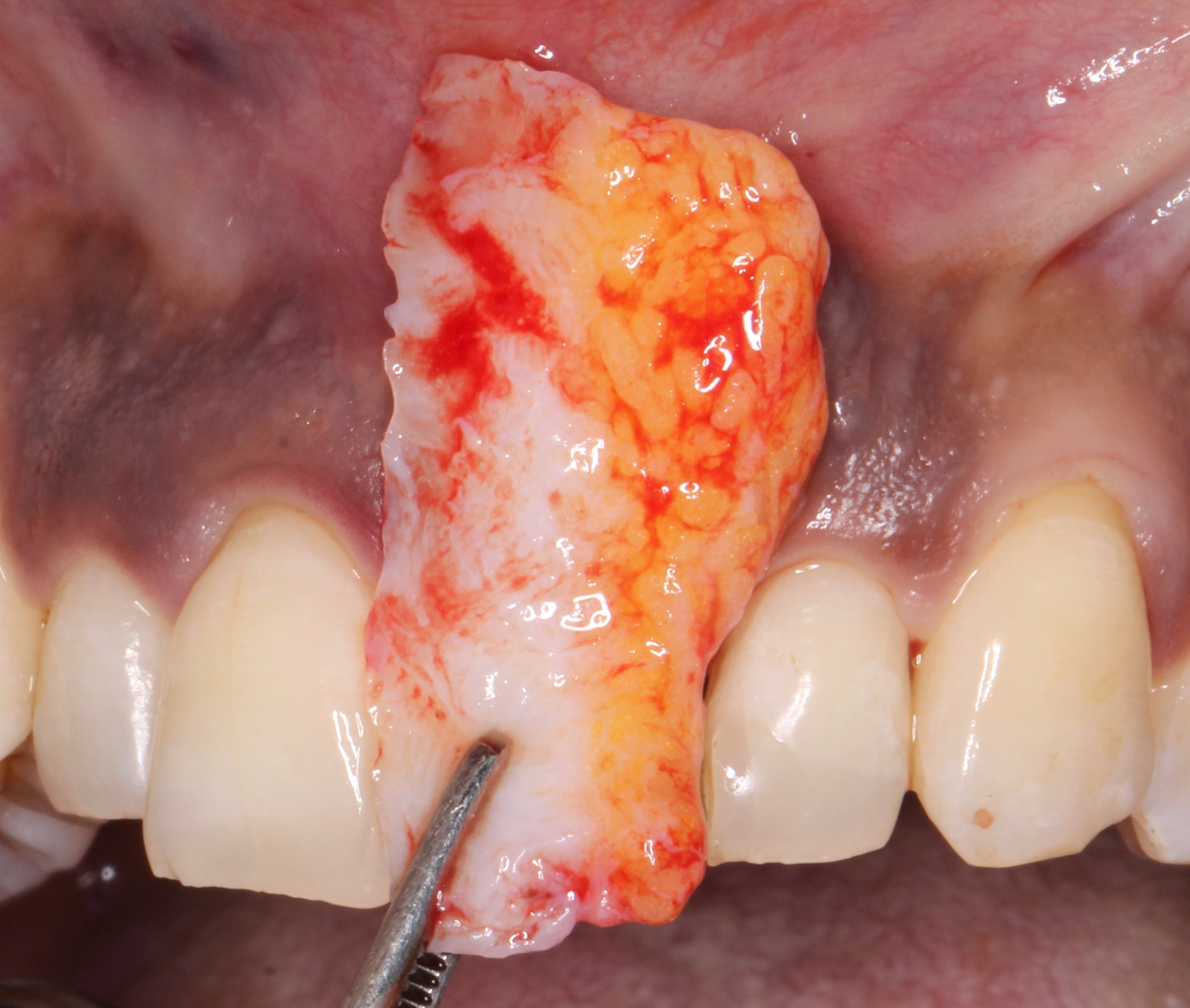
Figure 7.
A connective tissue graft was harvested from the palate and placed inside the defect ad modum “saddle” from the buccal aspect through the exposed coronal part to the palatal aspect.
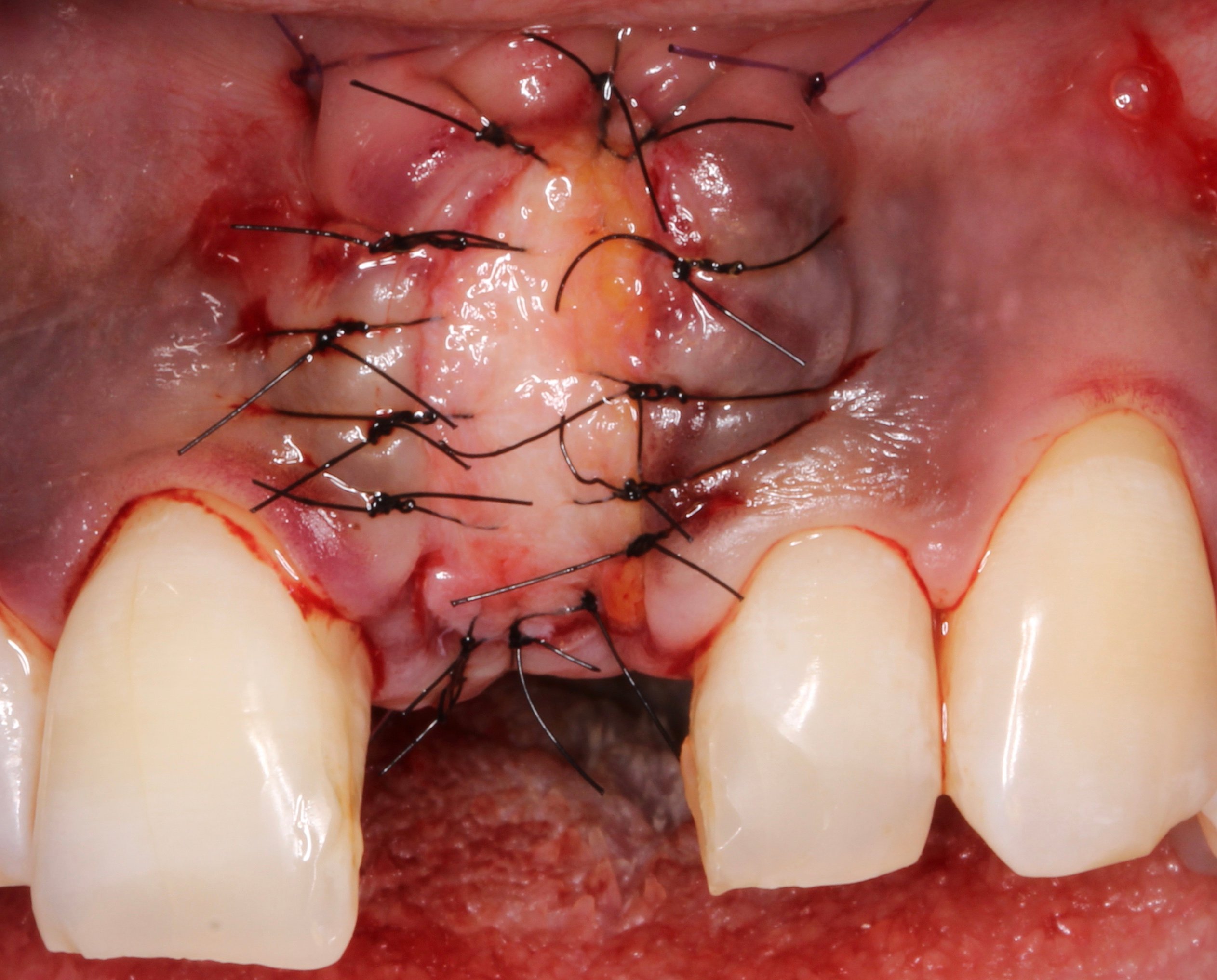
Figure 8.
A connective tissue graft was harvested from the palate and placed inside the defect ad modum “saddle” from the buccal aspect through the exposed coronal part to the palatal aspect.

Figure 9.
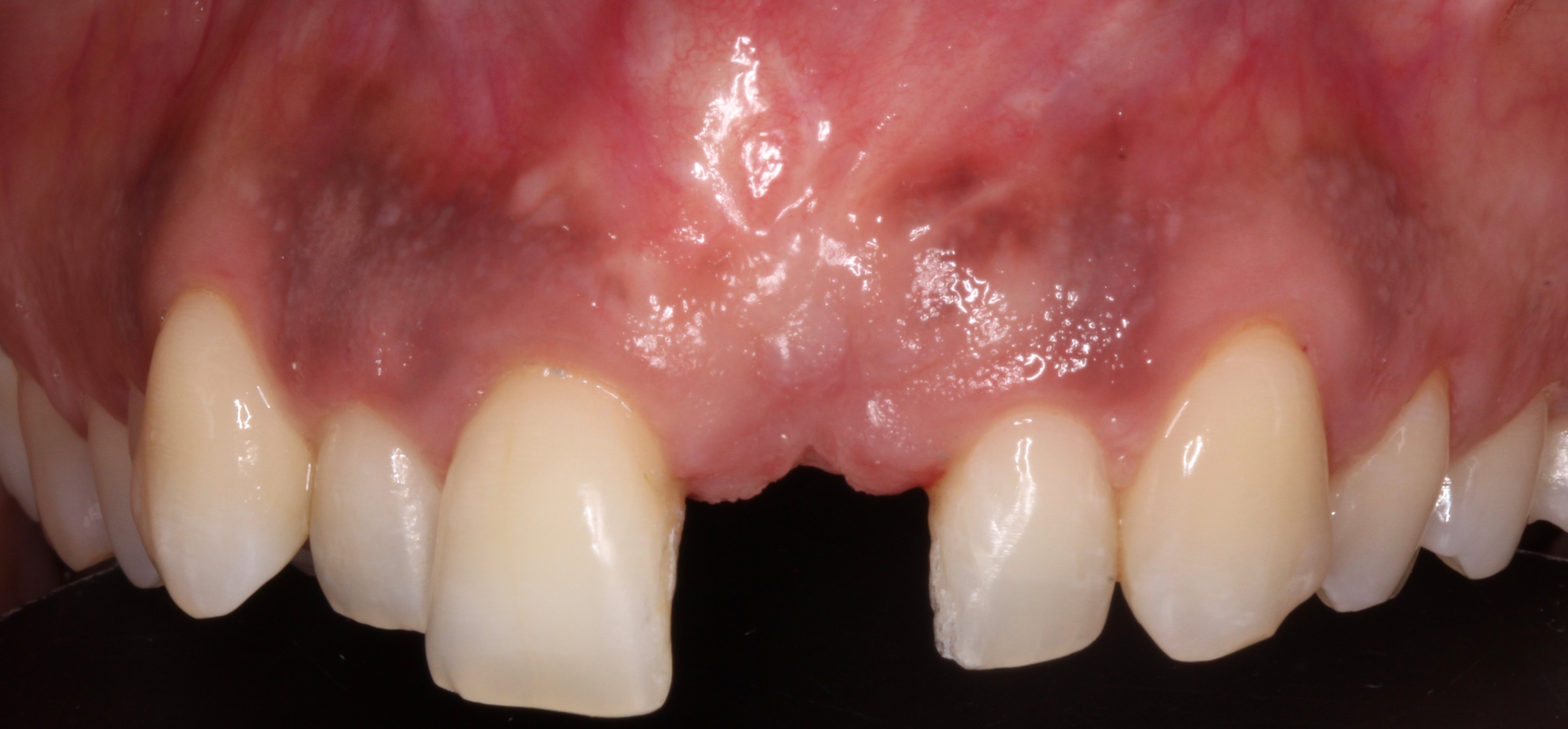
Figure 10.

Figure 11.

Figure 12.
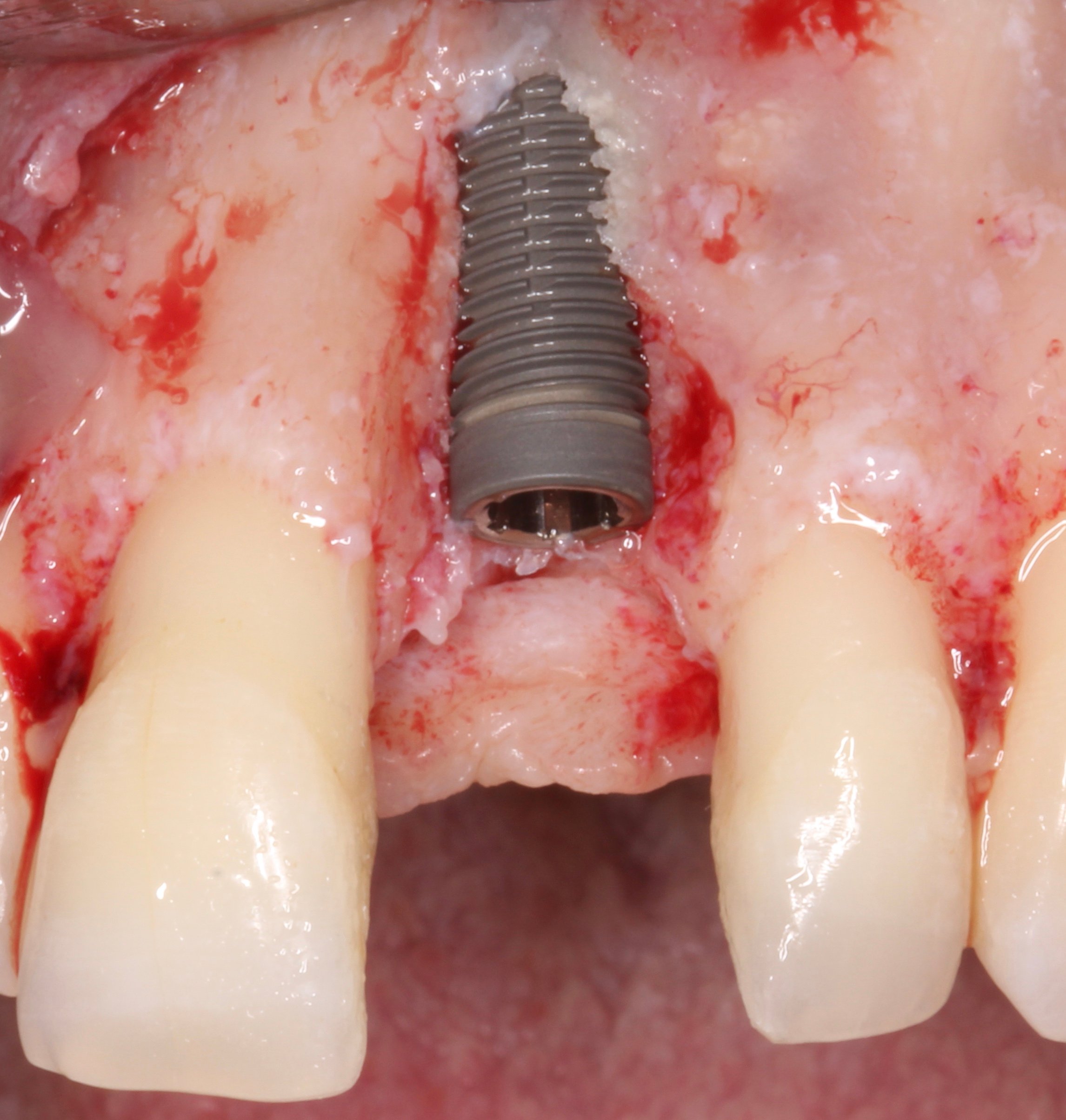
Figure 13.
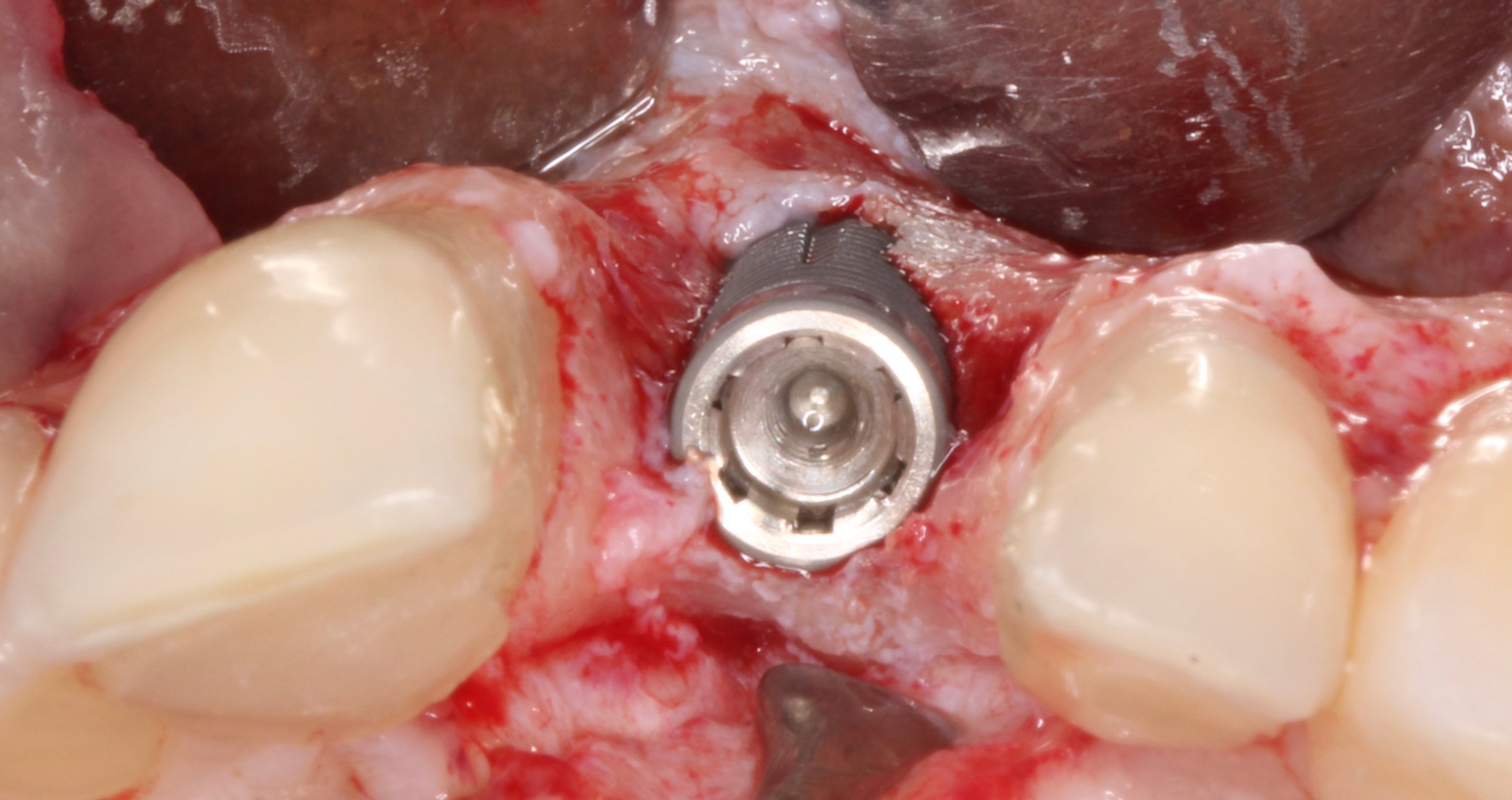
Figure 14.
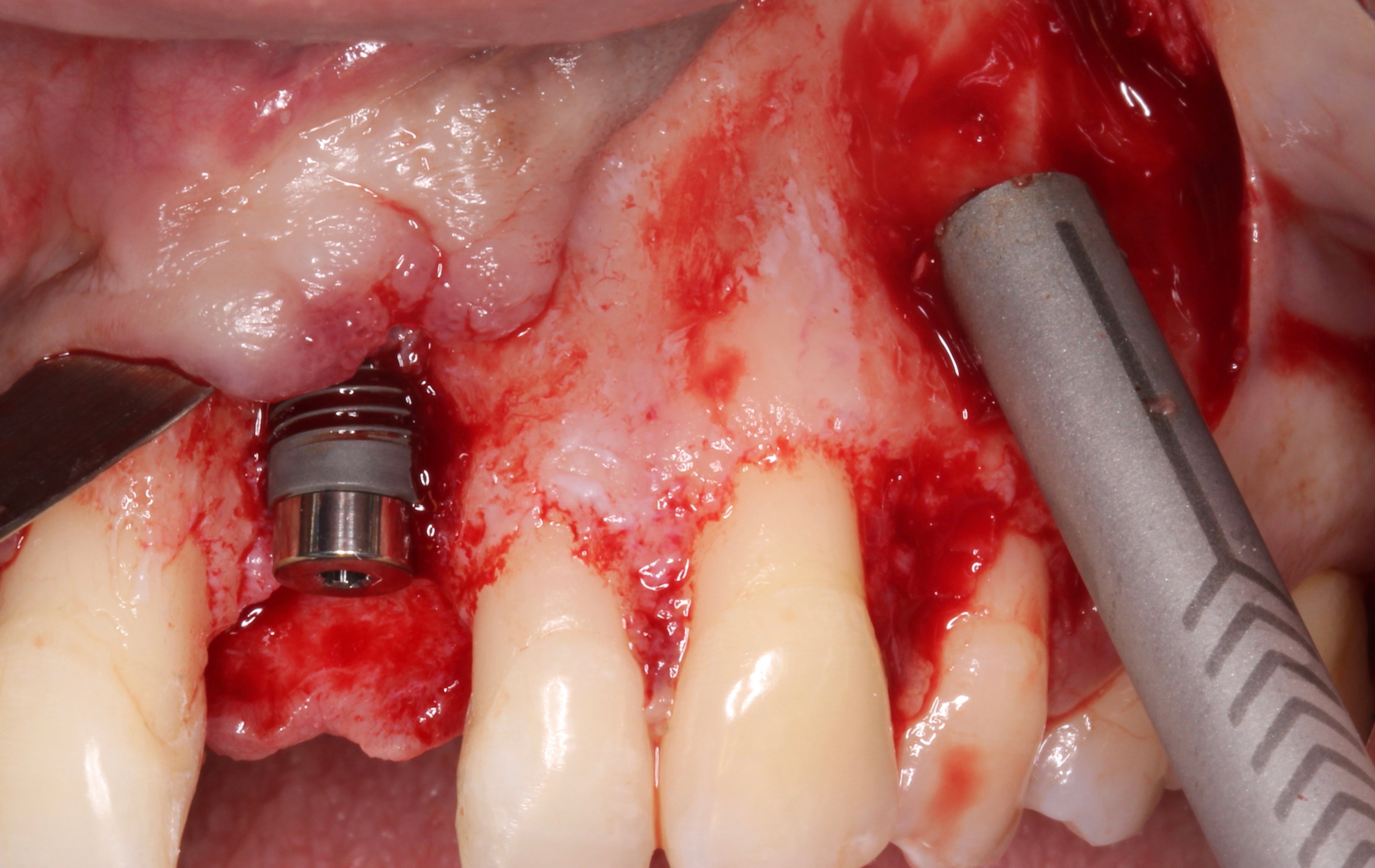
Figure 15.
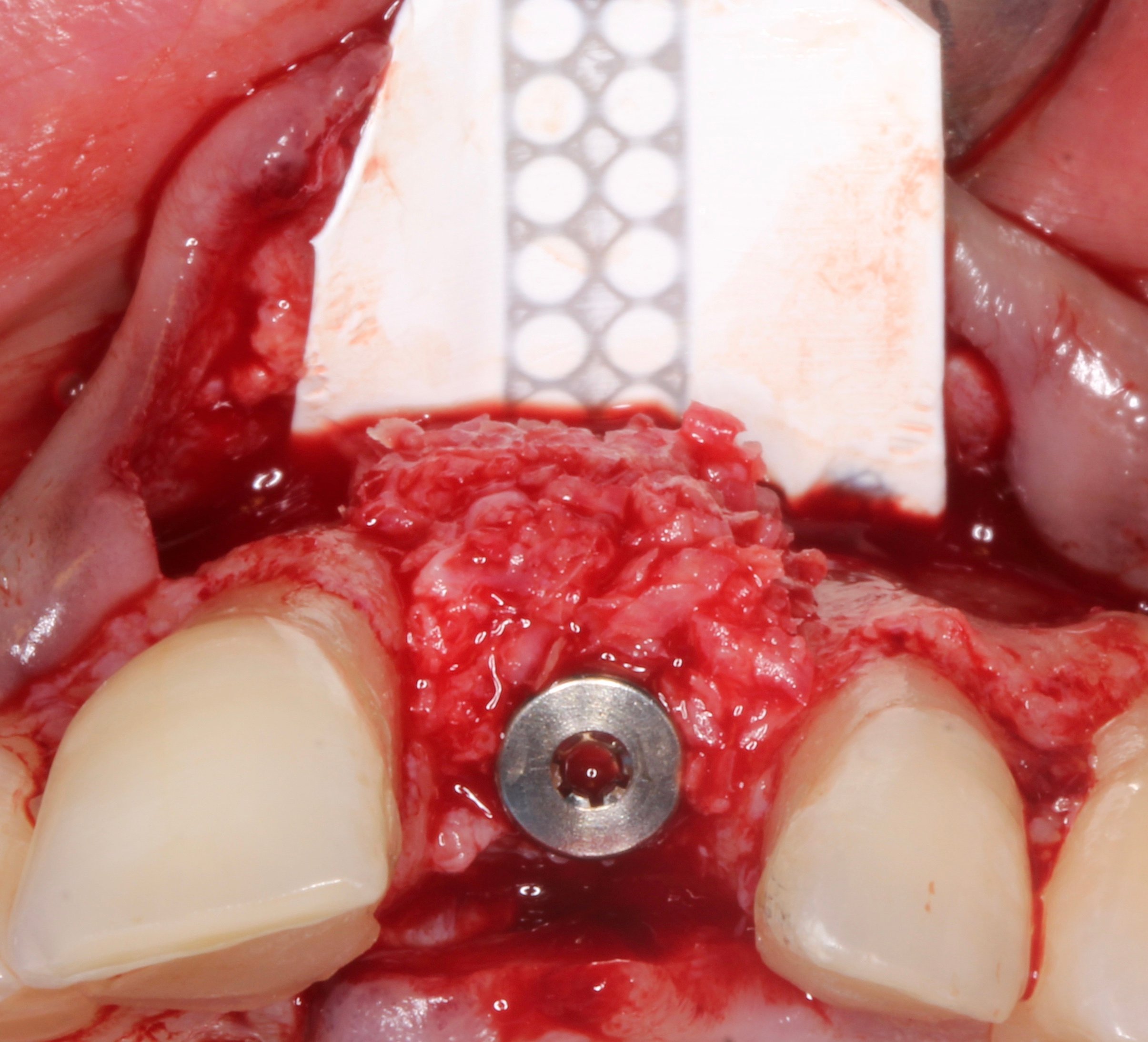
Figure 16.
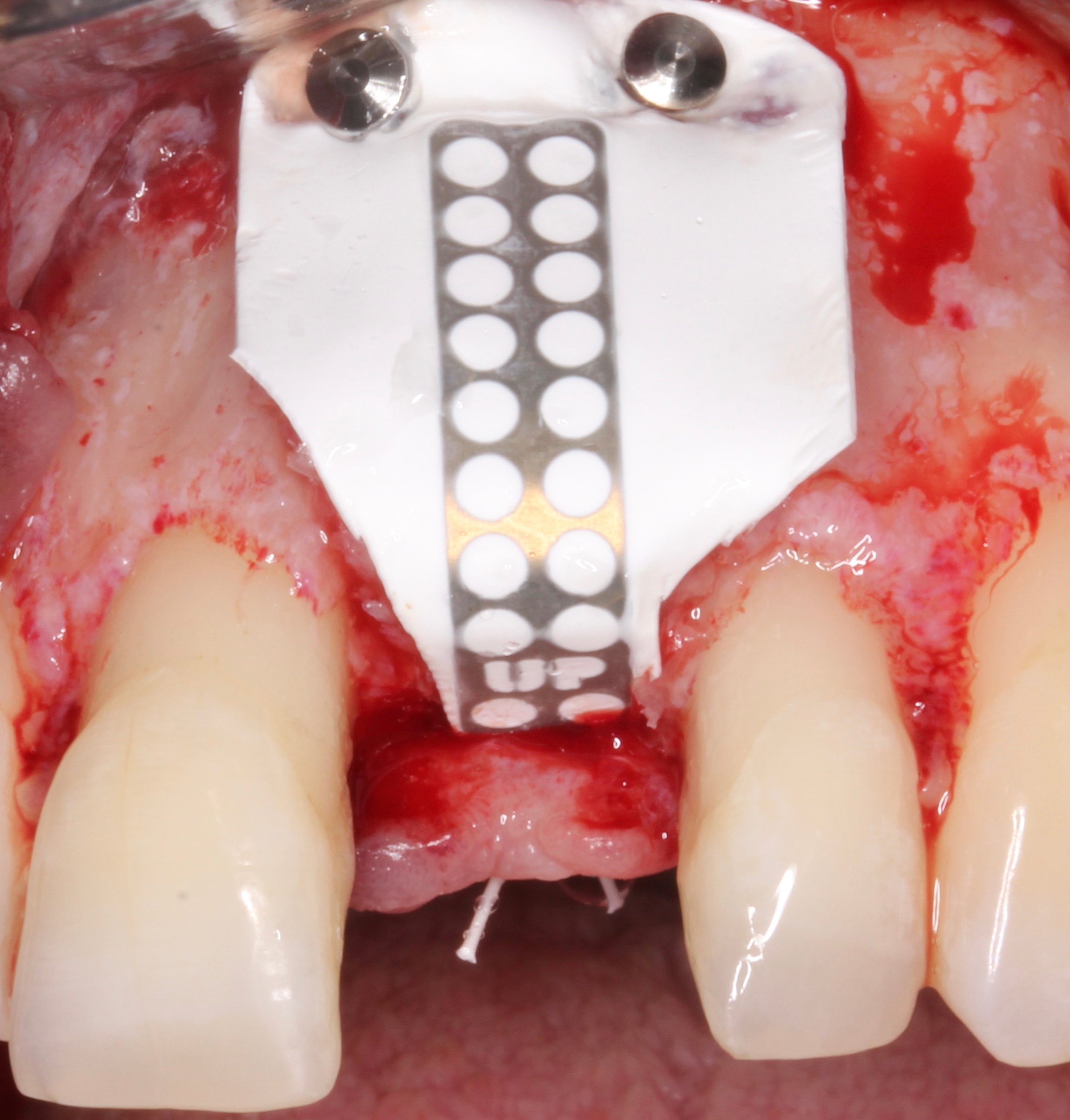
Figure 17.
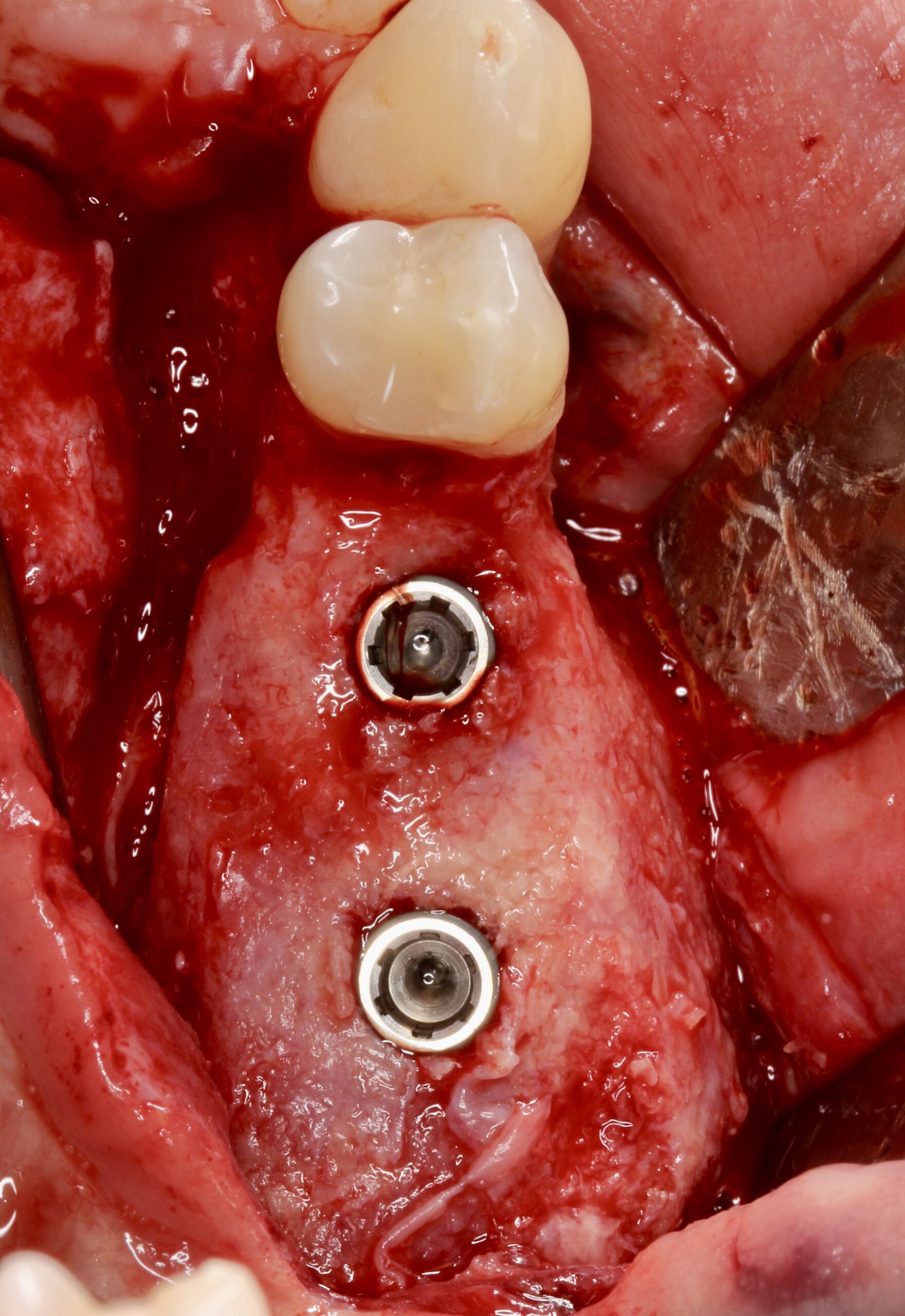
Figure 18.

Figure 19.
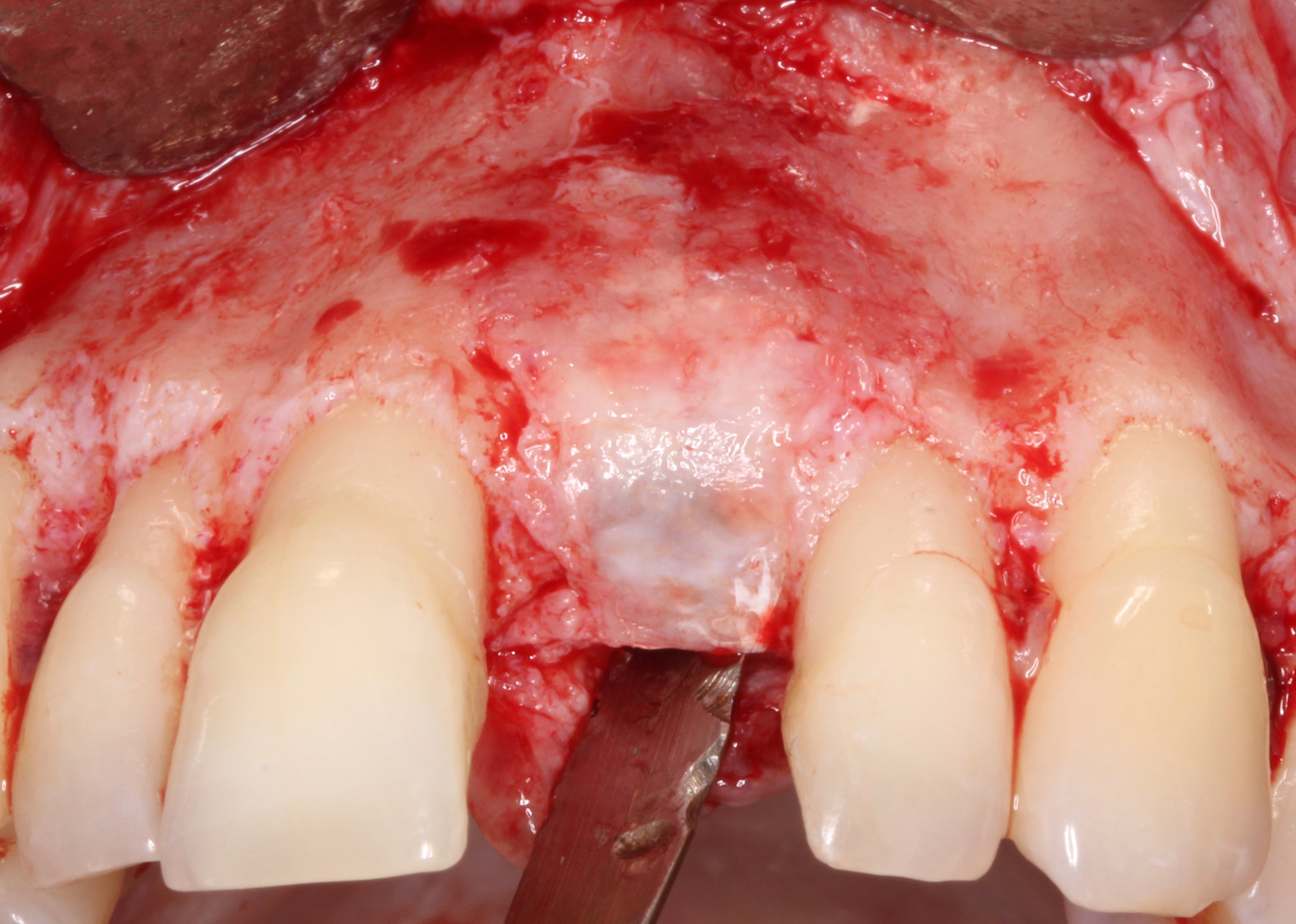
Figure 20.
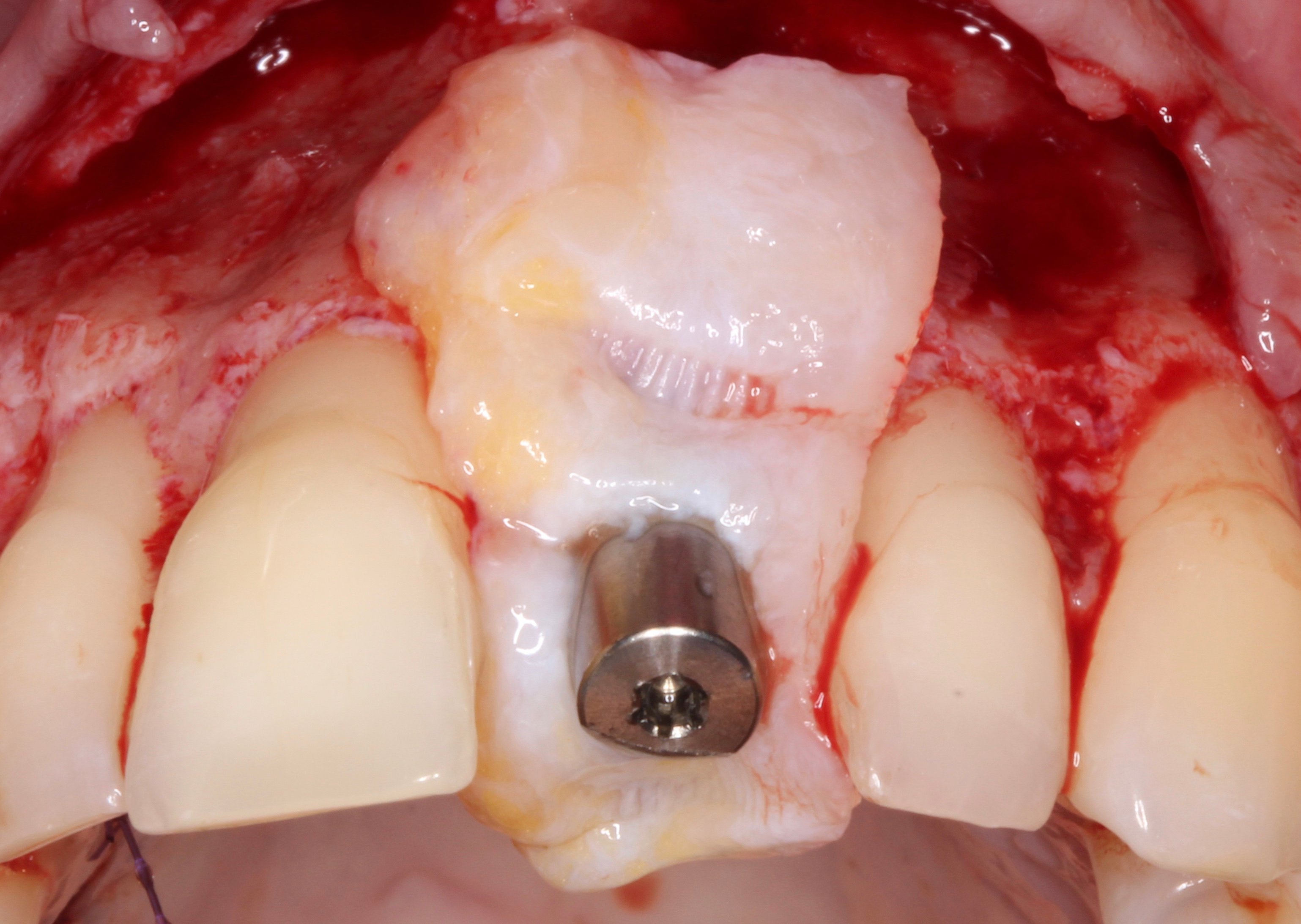
Figure 21.
A connective tissue graft was placed ad modum “poncho” around a 8 mm healing abutment.

Figure 22.

Figure 23.
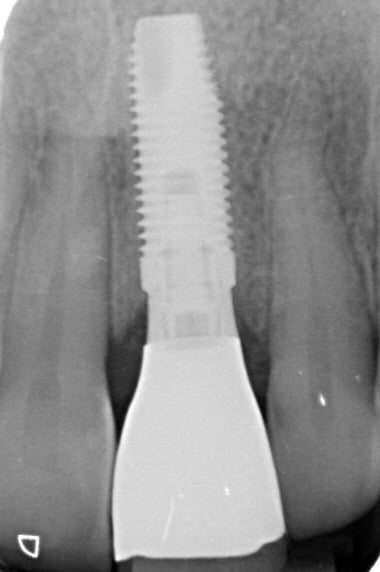
Figure 24.

