
Clinical Case: NeoGen® PTFE Membran, Neoss ProActive® Implants
3D GBR on the posterior maxilla
using a PTFE, Ti-reinforced NeoGen® membrane, 100% autogenous bone and Neoss ProActive® Implants
Dr. David González
DDS, M.Sc, PhD Master in Periodontics EFP and PhD Doctor at Complutense University of Madrid.
Private practice at Clínica Ortoperio in Murcia, Spain.
Facts
Patient:
38 years old woman, non-smoker, medically healthy.
Clinical problem:
Patient presented bone atrophy at right posterior maxilla missing 16 and 17.
Clinical solution:
After 1 year of implant-supported screw-retained crowns delivery hard and soft tissue stability was observed and an proper appearance was achieved.
Treatment plan:
- Patient was referred due to severe bone atrophy caused by gravis periimplantitis and history of periapical endodontic lesions on both molars.
- 9 months later: after seeing by a CBCT that localised bone atrophy did not allow to place implants a GBR procedure was performed using a dual PTFE, Ti-reinforced, NeoGen® membrane which was fixed by Neoss® tacks at buccal aspect and 3 Neoss® bonyscrews at palatal side. 100% autogenous bone was used as a filling material. Primary tension-free closure was achieved and healing was uneventful.
- 12 months later: Reentry was carried out, removing the membrane and placing 2 Neoss® implants.
- 2 months later: a Free Gingival Graft was placed at buccal aspect to reposition the mucogingival line and to create a band of keratinised mucosa.
- 2 months later: 2 screw-retained zirconia-porcelane crowns were delivered.
- 1 year later: Clinical and radiographic status of the implants was healthy.
Products:
1 NeoGen Ti-Reinforced PTFE Membrane.
Conclusion:
3D GBR using a dual-PTFE, Ti-reinforced NeoGen® membrane and 100% autogenous bone is a fully predictable treatment for the severe bone atrophy on the posterior maxilla.
Step by step
Step by step

Figure 1.
Clinical view of the right posterior maxilla showing severe bone atrophy.
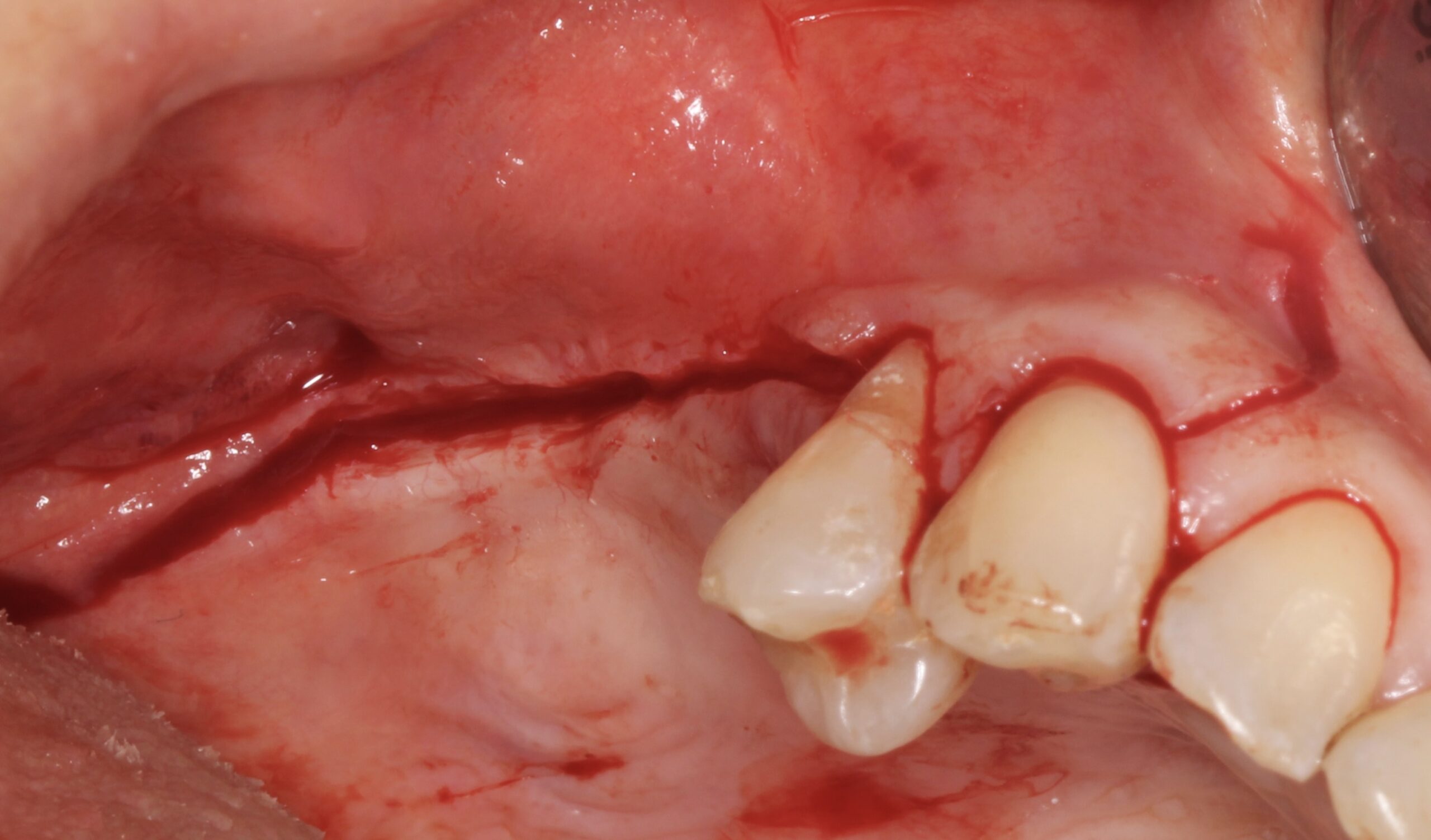
Figure 2.
Full thickness incision to expose the alveolar ridge.

Figure 3.
Severe vertical bone loss.

Figure 4.
Bone cortical cylinders were harvested from both external oblique lines and bone was also obtained by using bone scraper from both sides. The bone cylinders were crushed and mixed with the scraped bone.
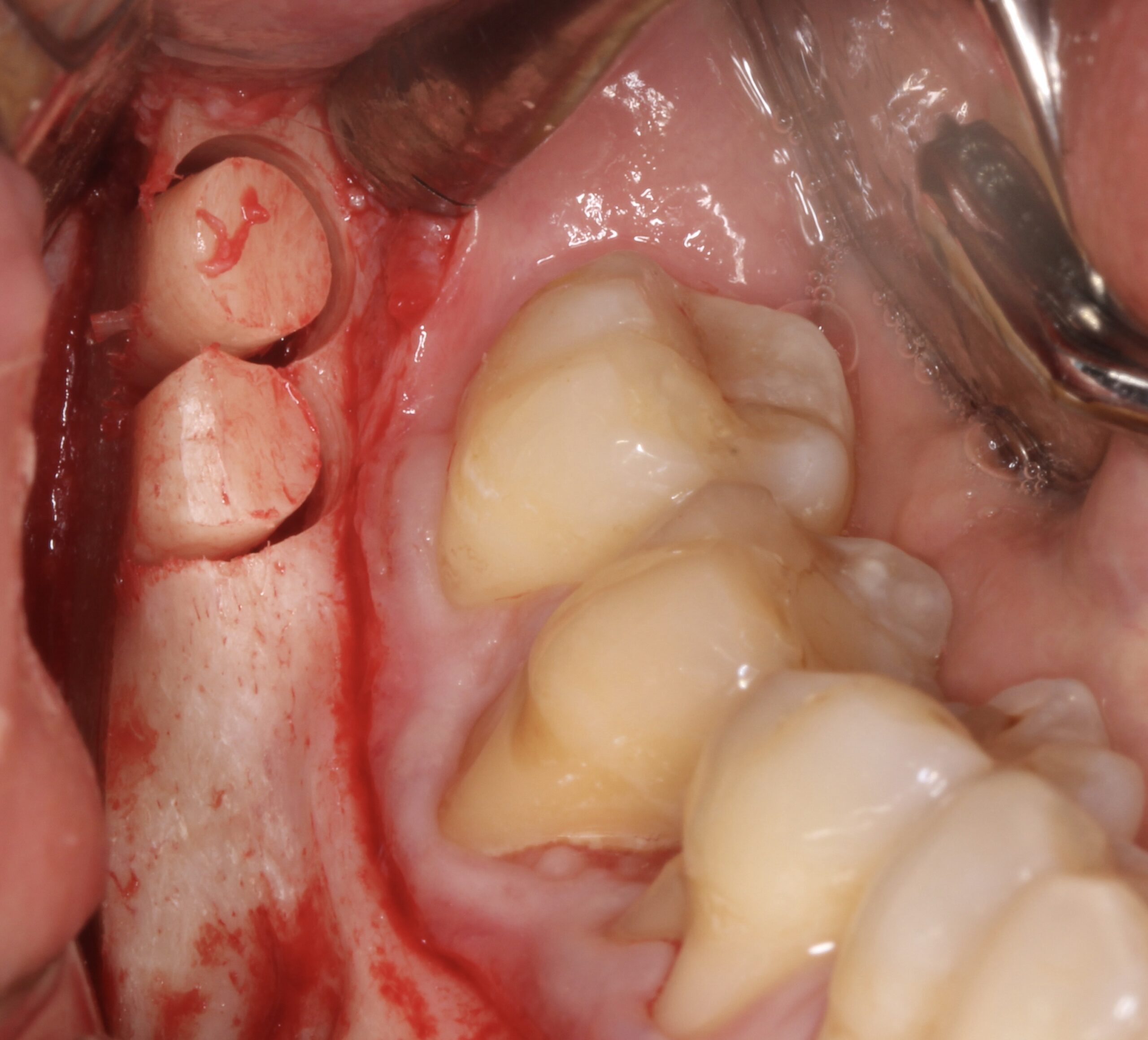
Figure 5.
Bone cortical cylinders were harvested from both external oblique lines and bone was also obtained by using bone scraper from both sides. The bone cylinders were crushed and mixed with the scraped bone.

Figure 6.
Bone cortical cylinders were harvested from both external oblique lines and bone was also obtained by using bone scraper from both sides. The bone cylinders were crushed and mixed with the scraped bone.
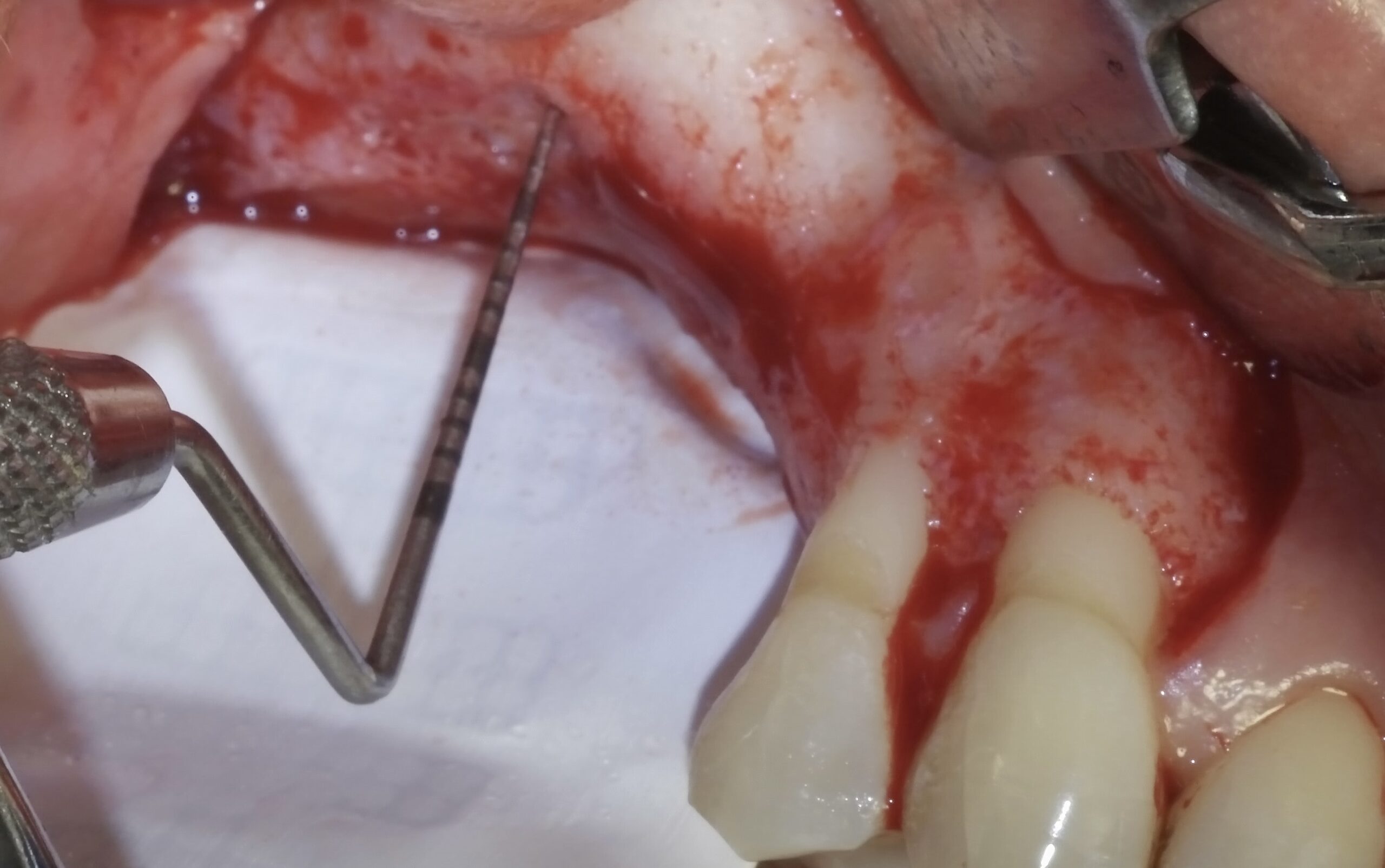
Figure 7.
A dual-PTFE, Ti-reinforced, NeoGen® membrane was fixed at palatal aspect by 3 Neoss® screws.

Figure 8.
All the harvested bone (scraped and particulated) was mixed and packed on the alveolar ridge.
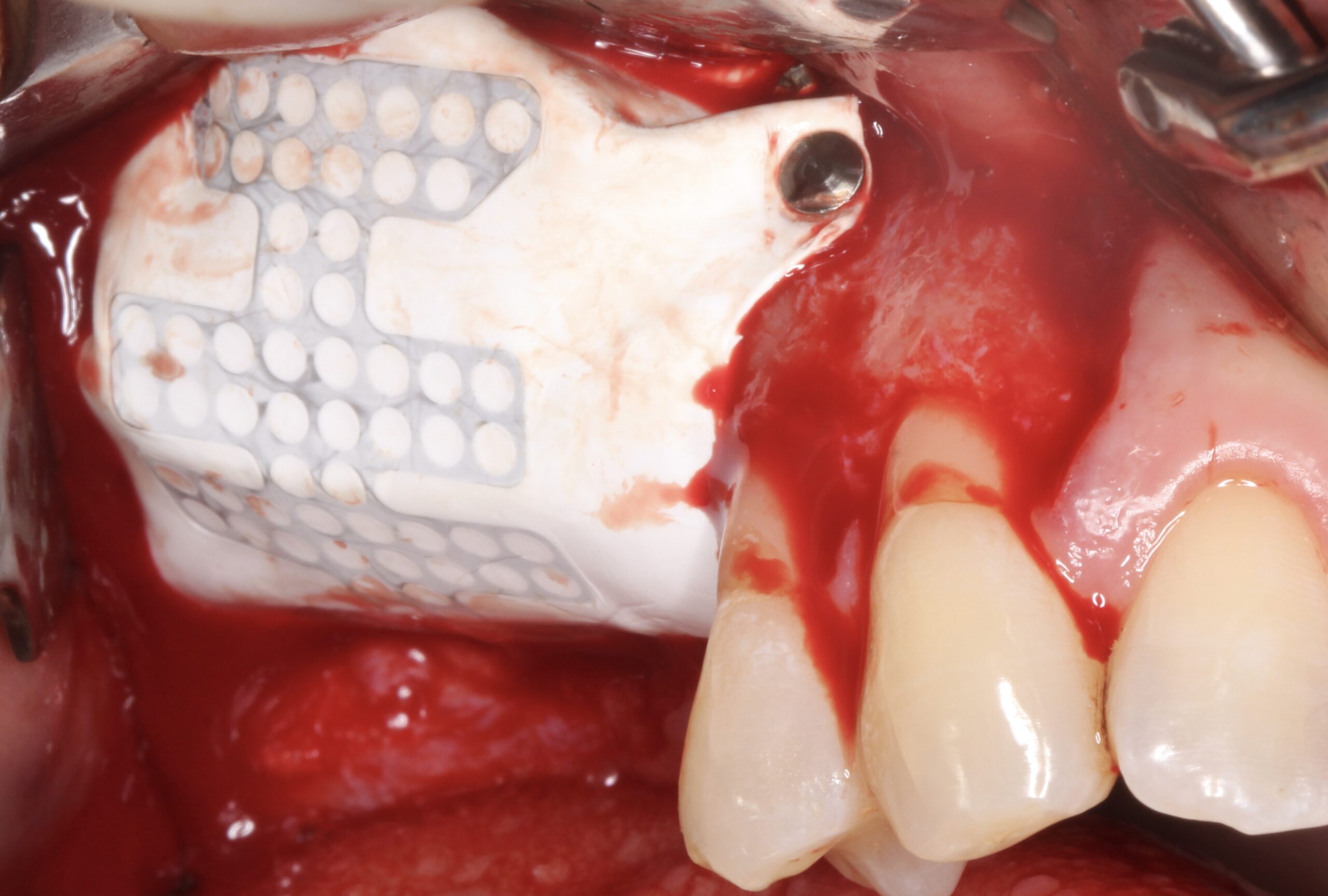
Figure 9.
The membrane was fixed with tacks at buccal aspect covering the ridge trying to gain the maximum possible from the distal bone peak to the maxillary tuberosity.
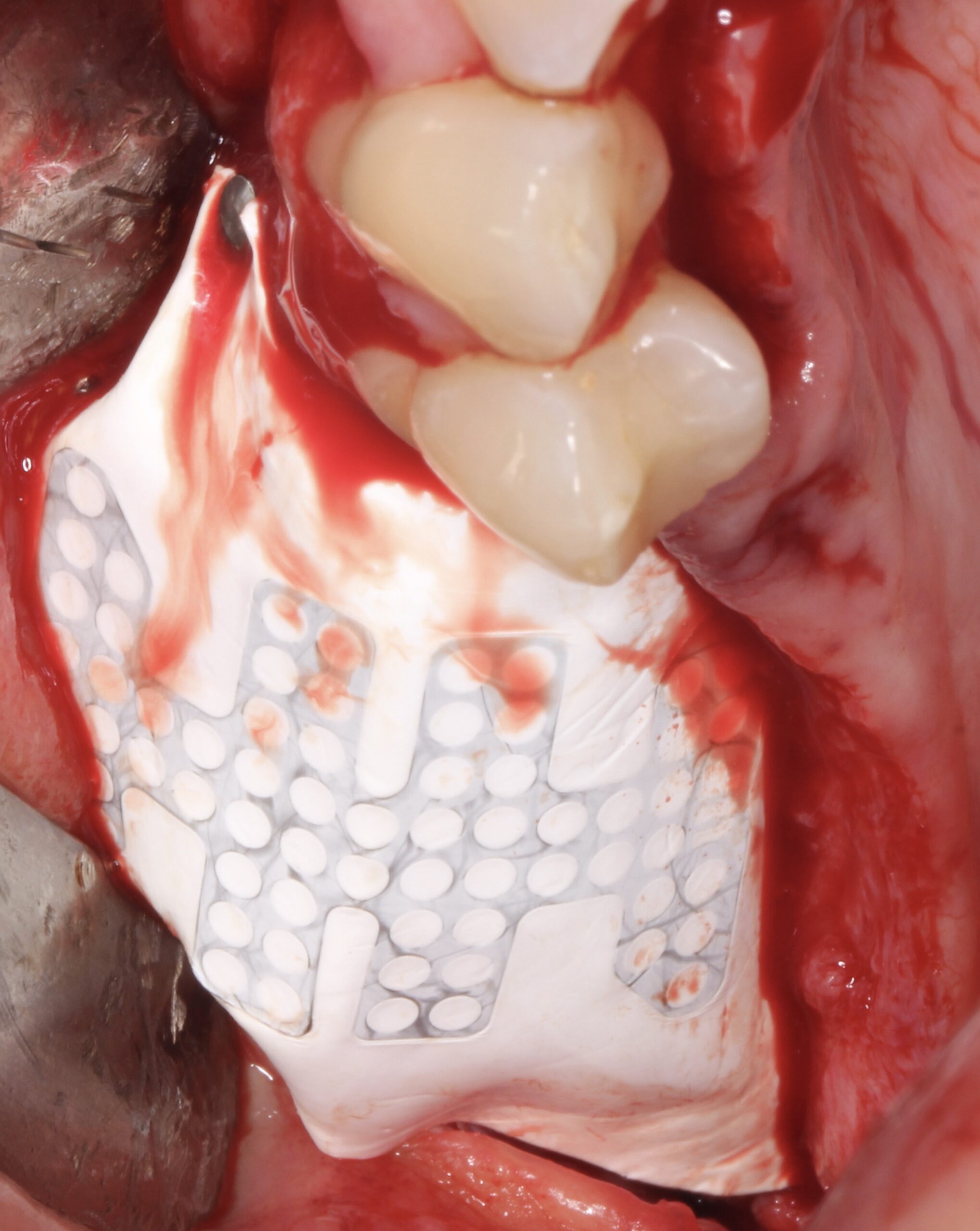
Figure 10.
The membrane was fixed with tacks at buccal aspect covering the ridge trying to gain the maximum possible from the distal bone peak to the maxillary tuberosity.
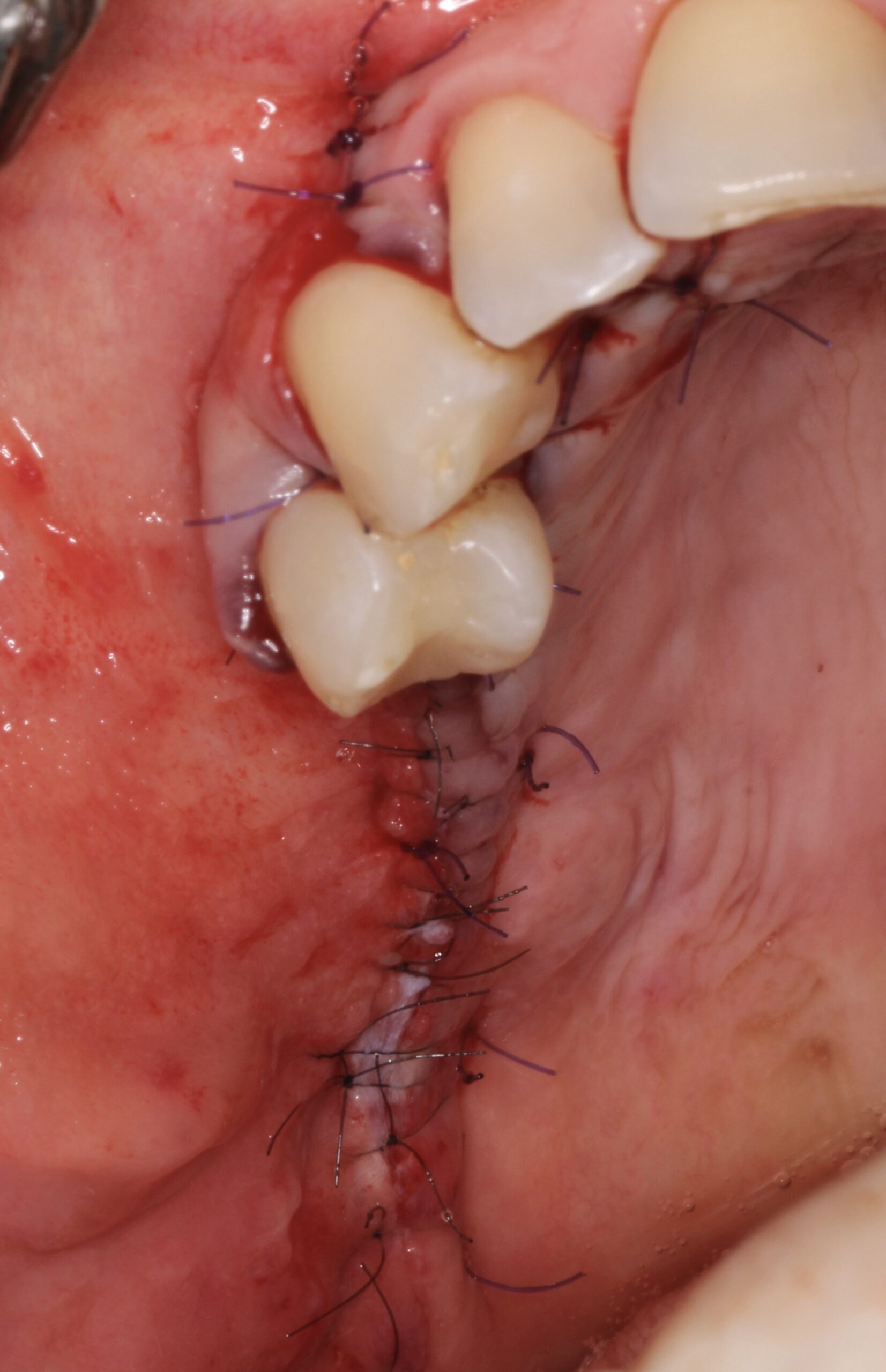
Figure 11.
After realising incisions on the periosteum, primary tension-free closure was achieved by mattress sutures and then interrupted sutures.

Figure 12.
1 year after the GBR surgery, reentry was carried out.
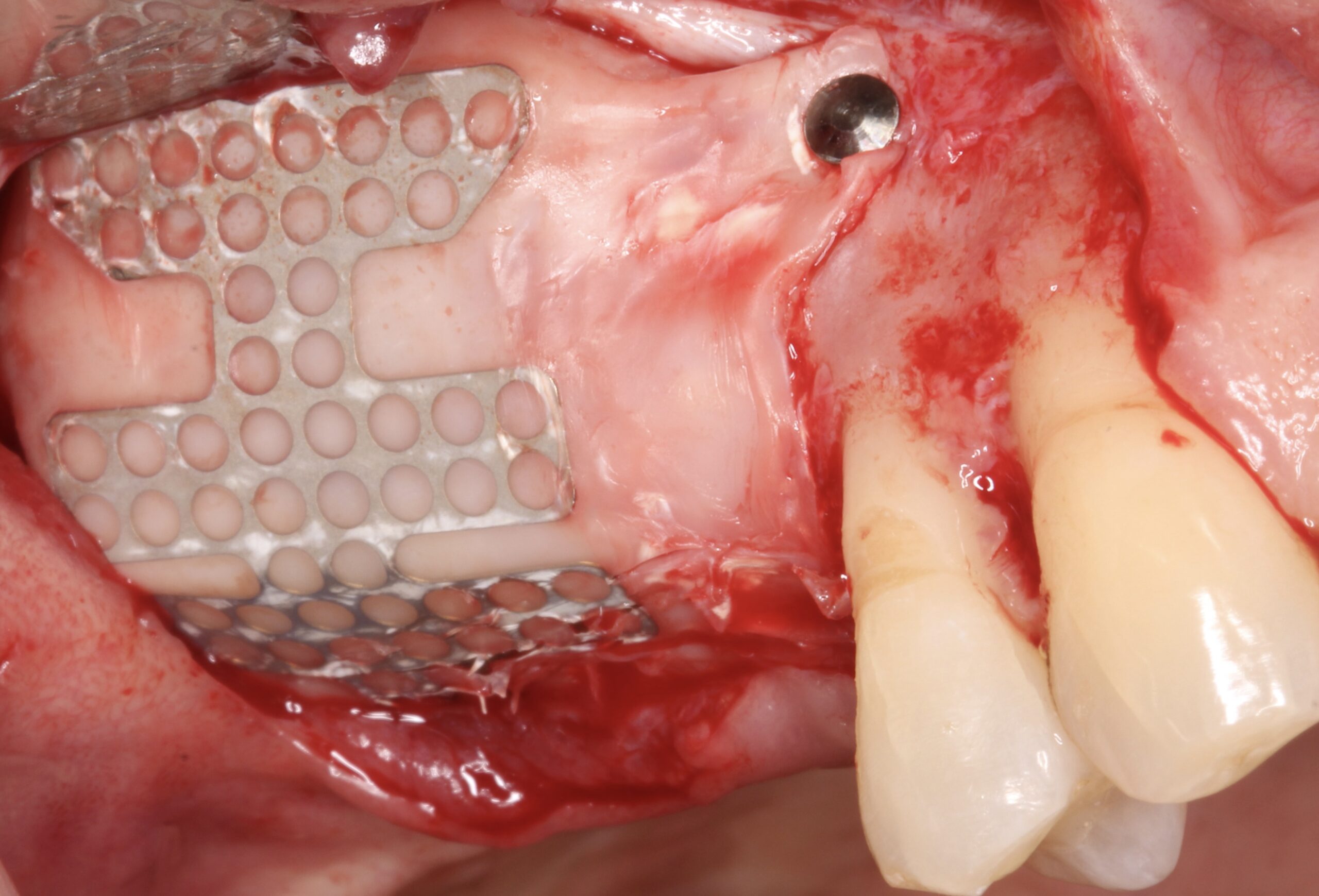
Figure 13.
After raising the flap, the membrane was firm at position.
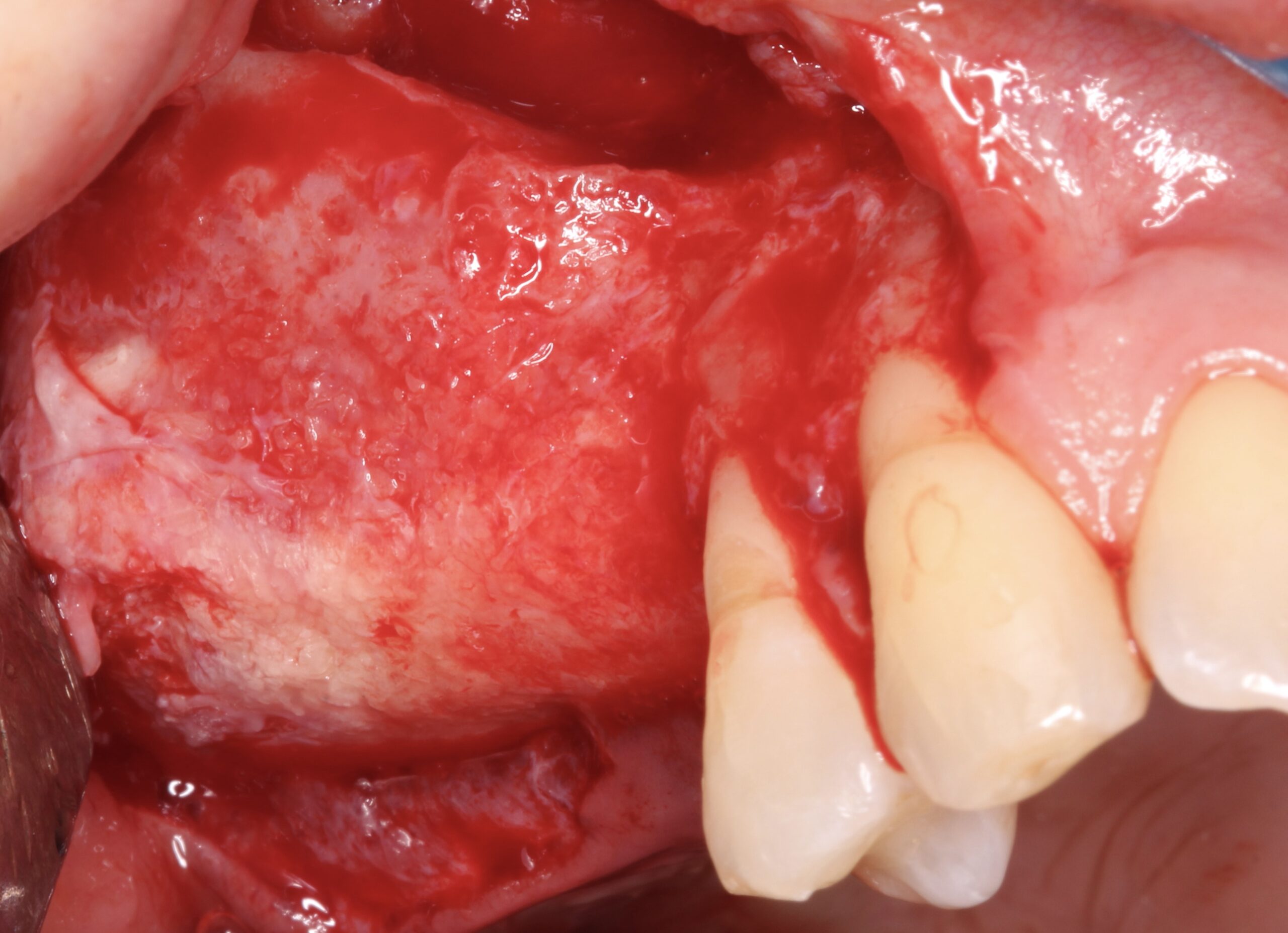
Figure 14.
After removing the membrane it was evident that complete 3D bone regeneration was achieved.
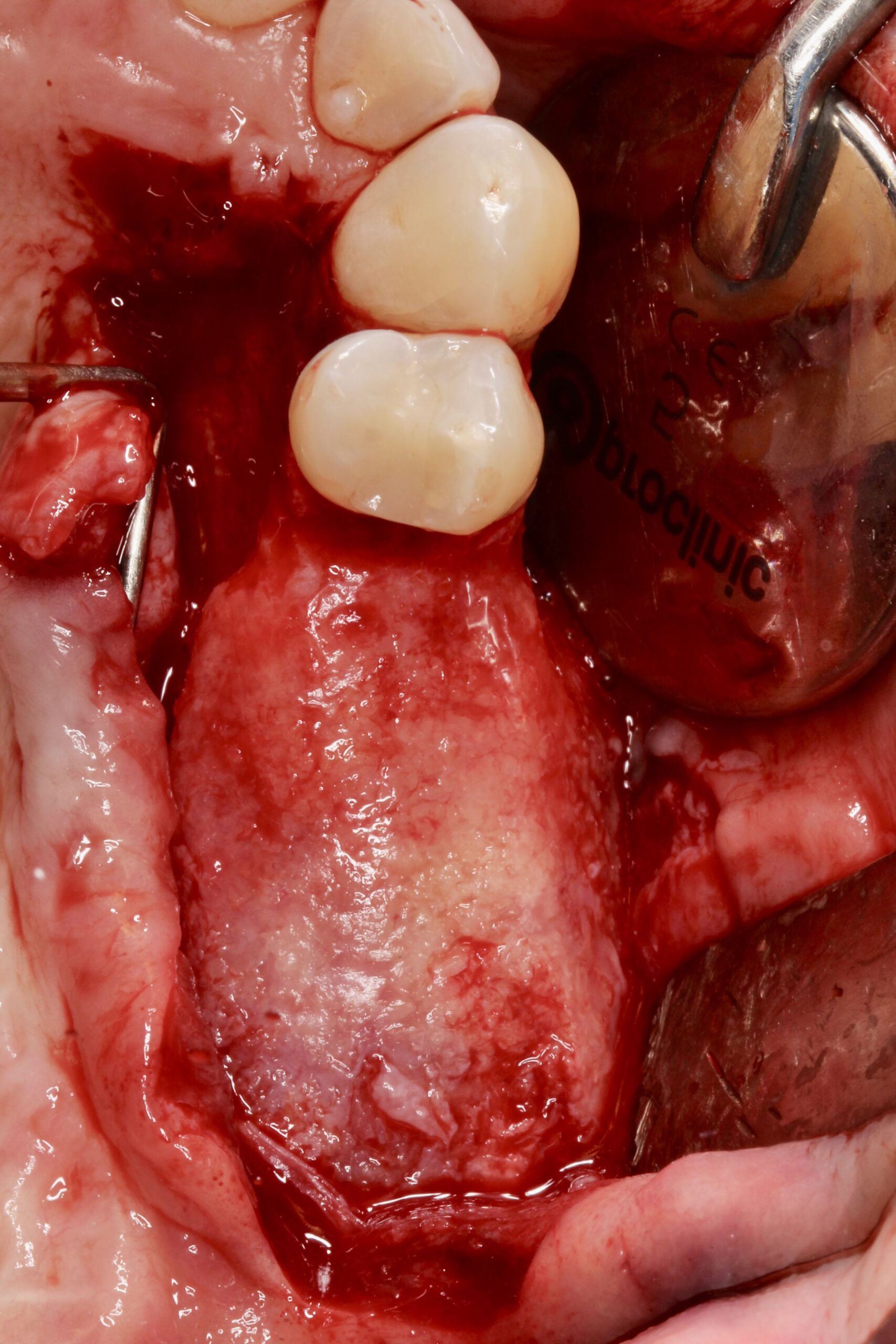
Figure 15.
After removing the membrane it was evident that complete 3D bone regeneration was achieved.
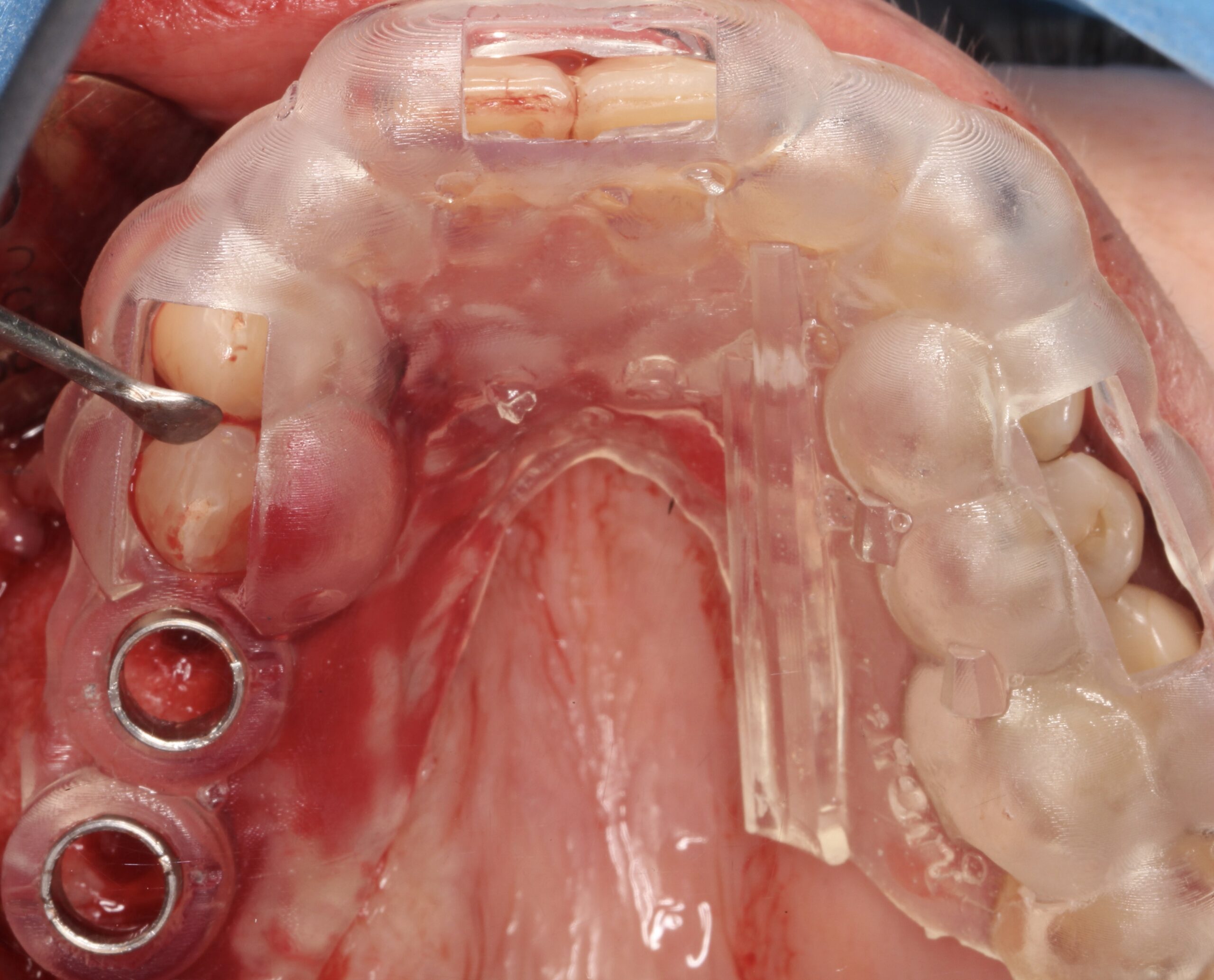
Figure 16.
Using a digital surgical guide.
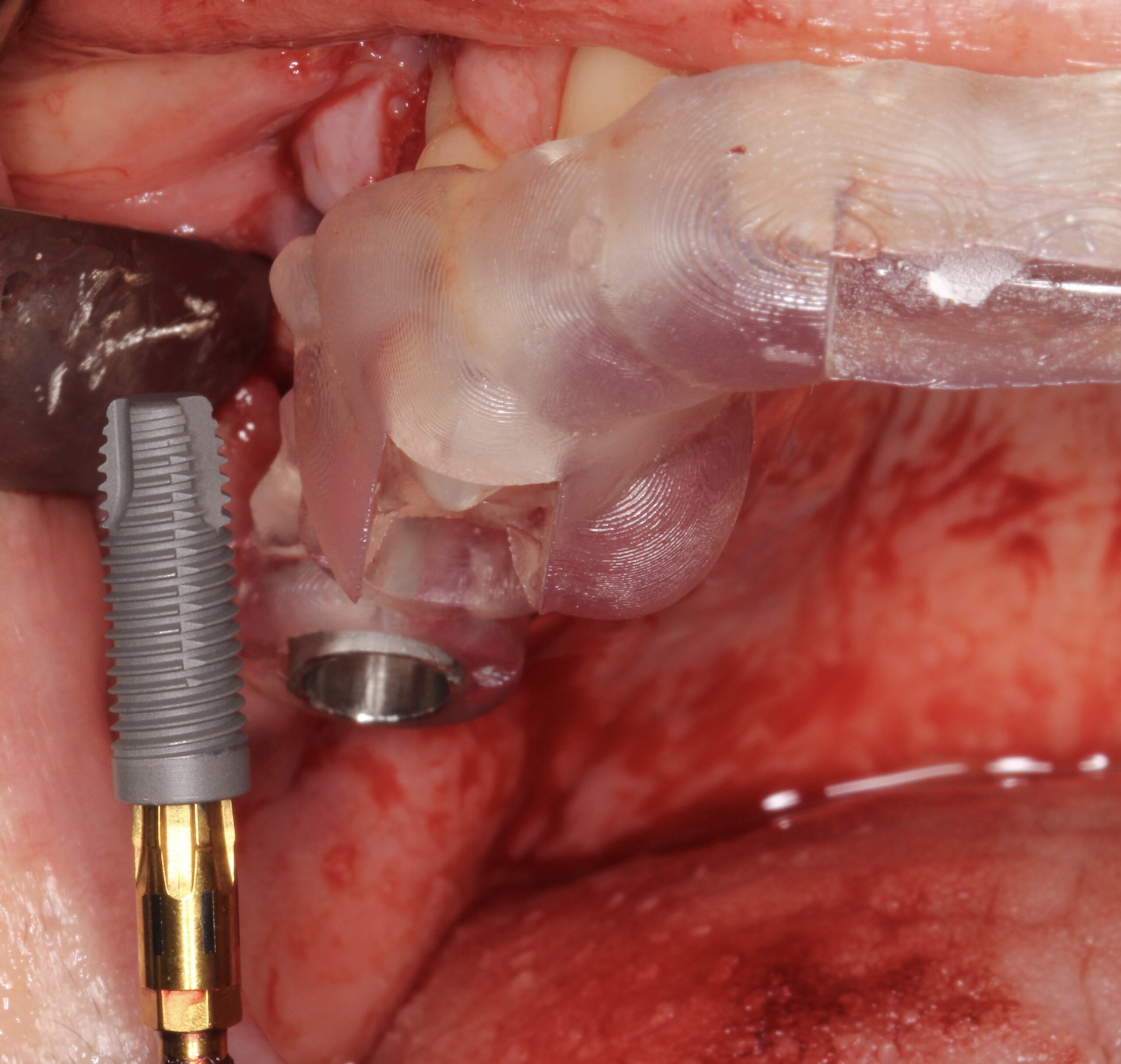
Figure 17.
Two 4.5 mm x 13 mm Neoss ProActive® implants were placed.
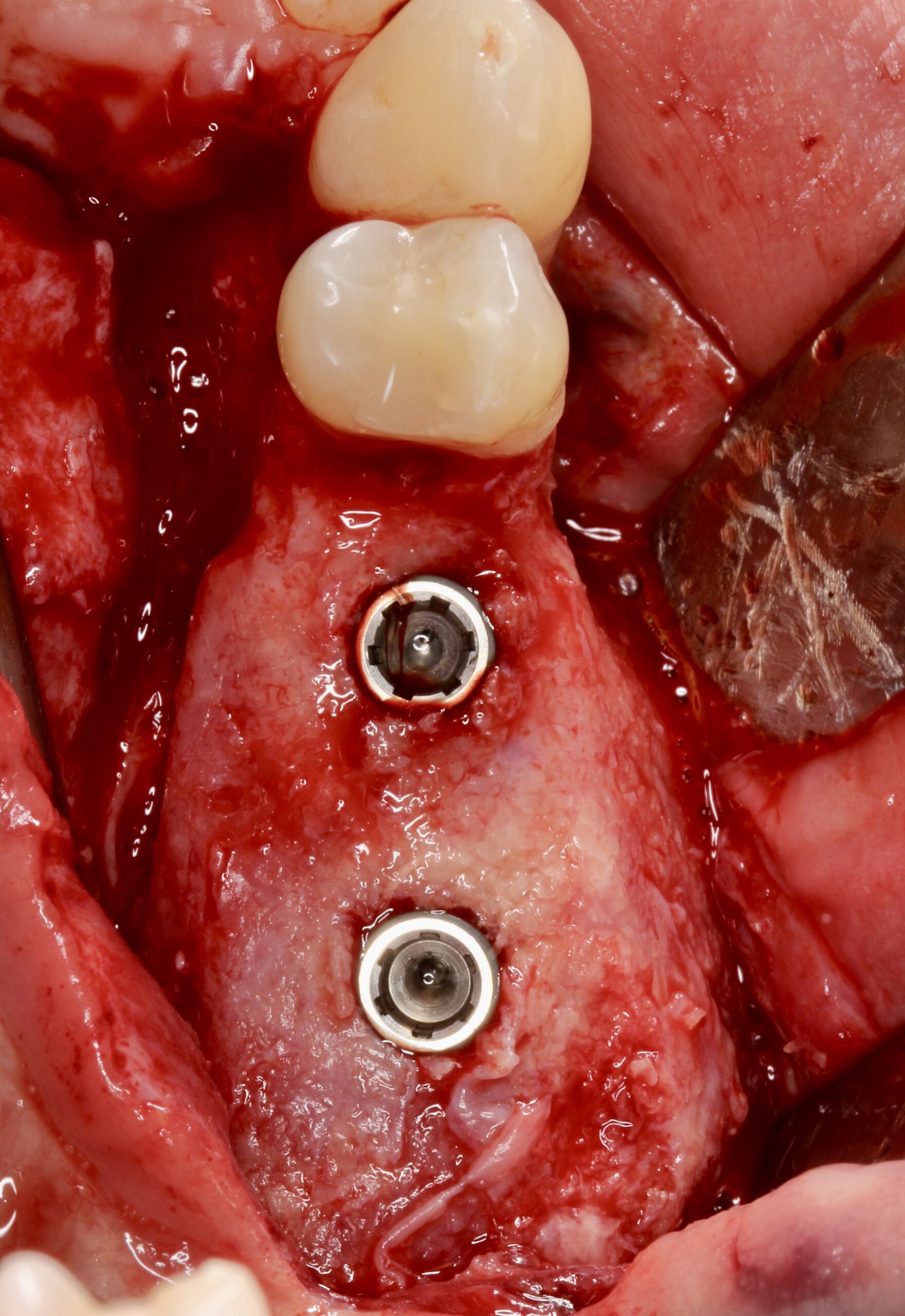
Figure 18.
Placed at 16 and 17 positions.
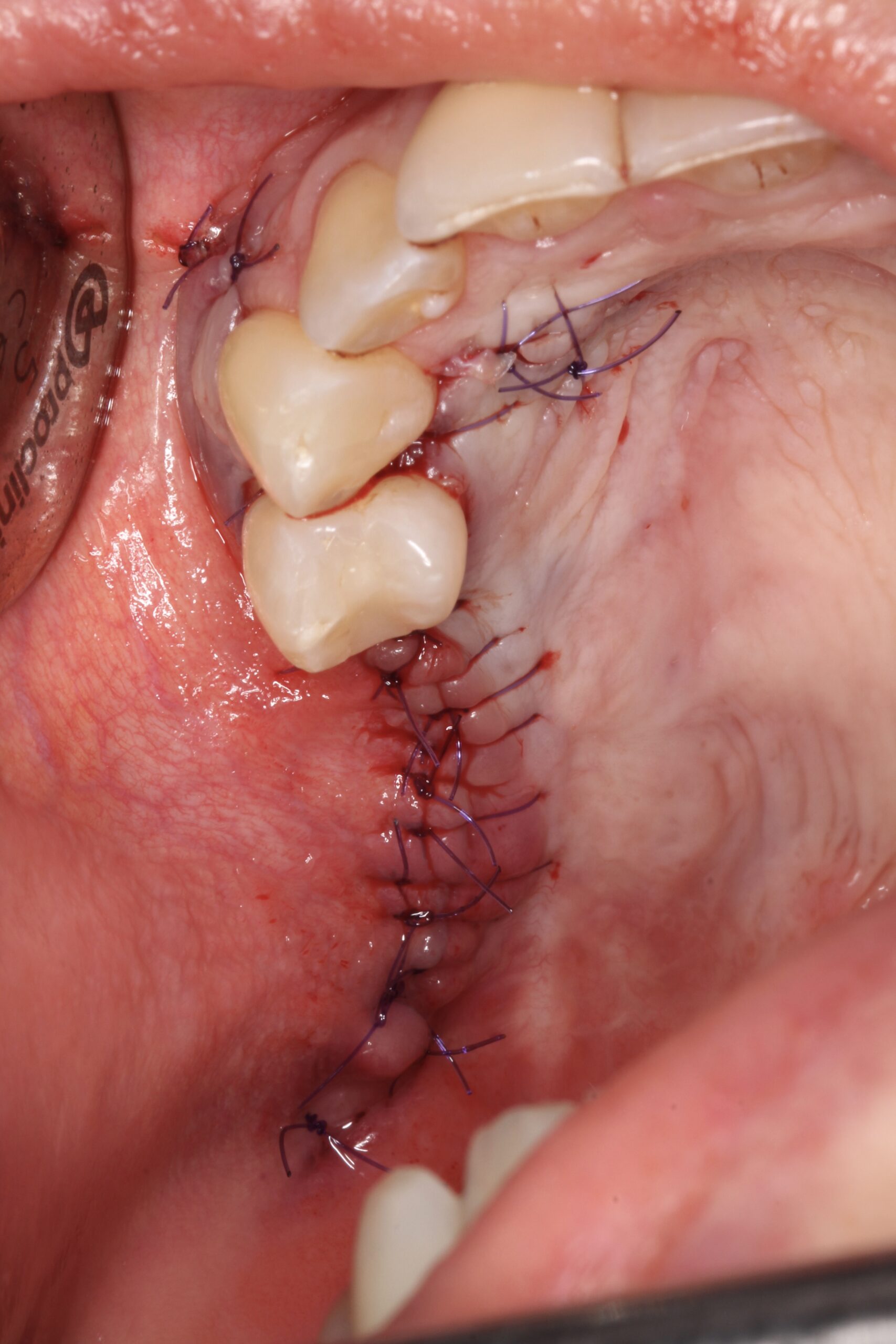
Figure 19.
The implants were submerged during healing osseointegration period.

Figure 20.
2 months later it was evident that there was no keratinised mucosa at buccal aspect and in fact even on the supracrestal area lack of keratinised mucosa was observed.
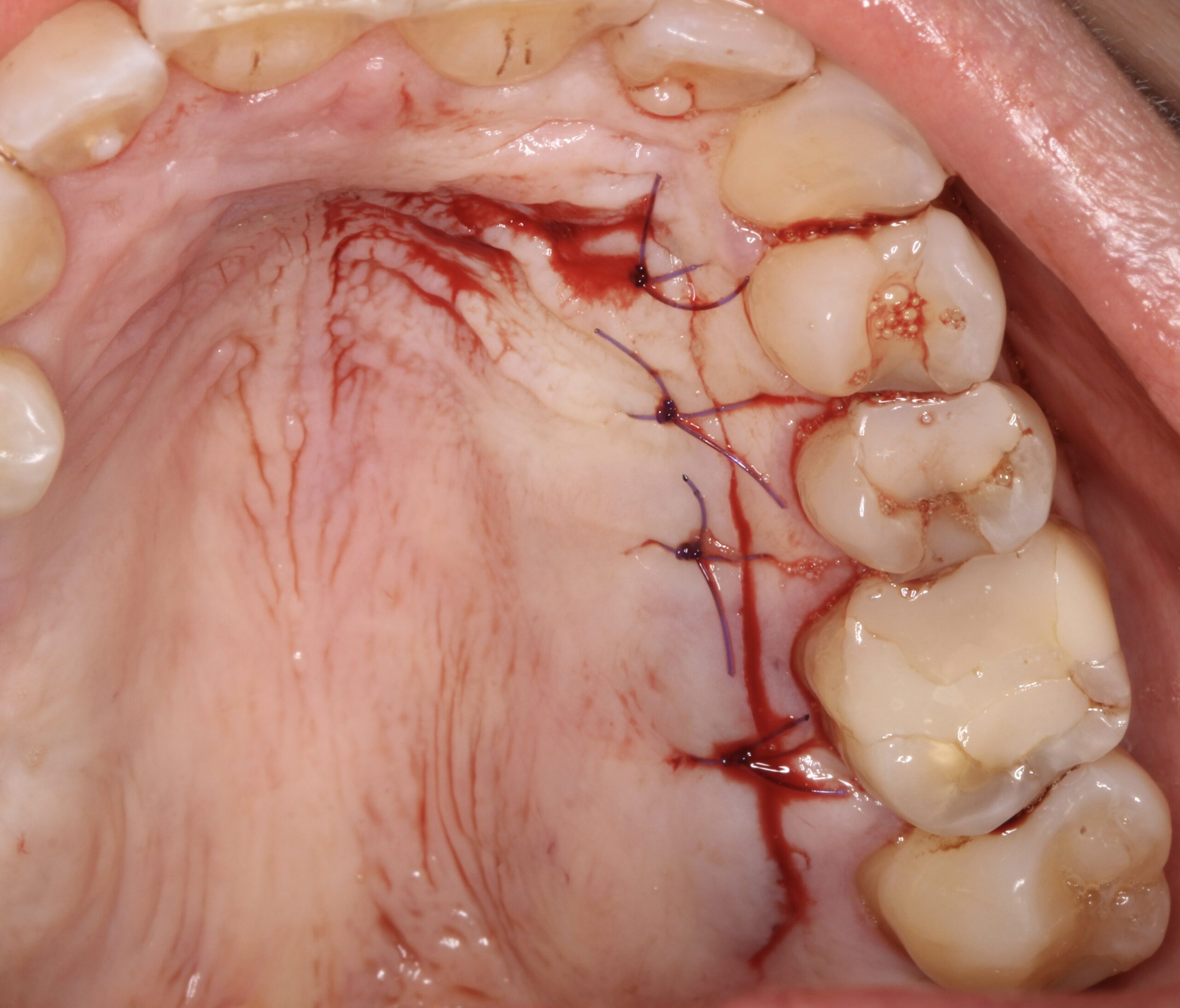
Figure 21.
A connective tissue graft was harvested using a trap-door from the contralateral side of the palate.
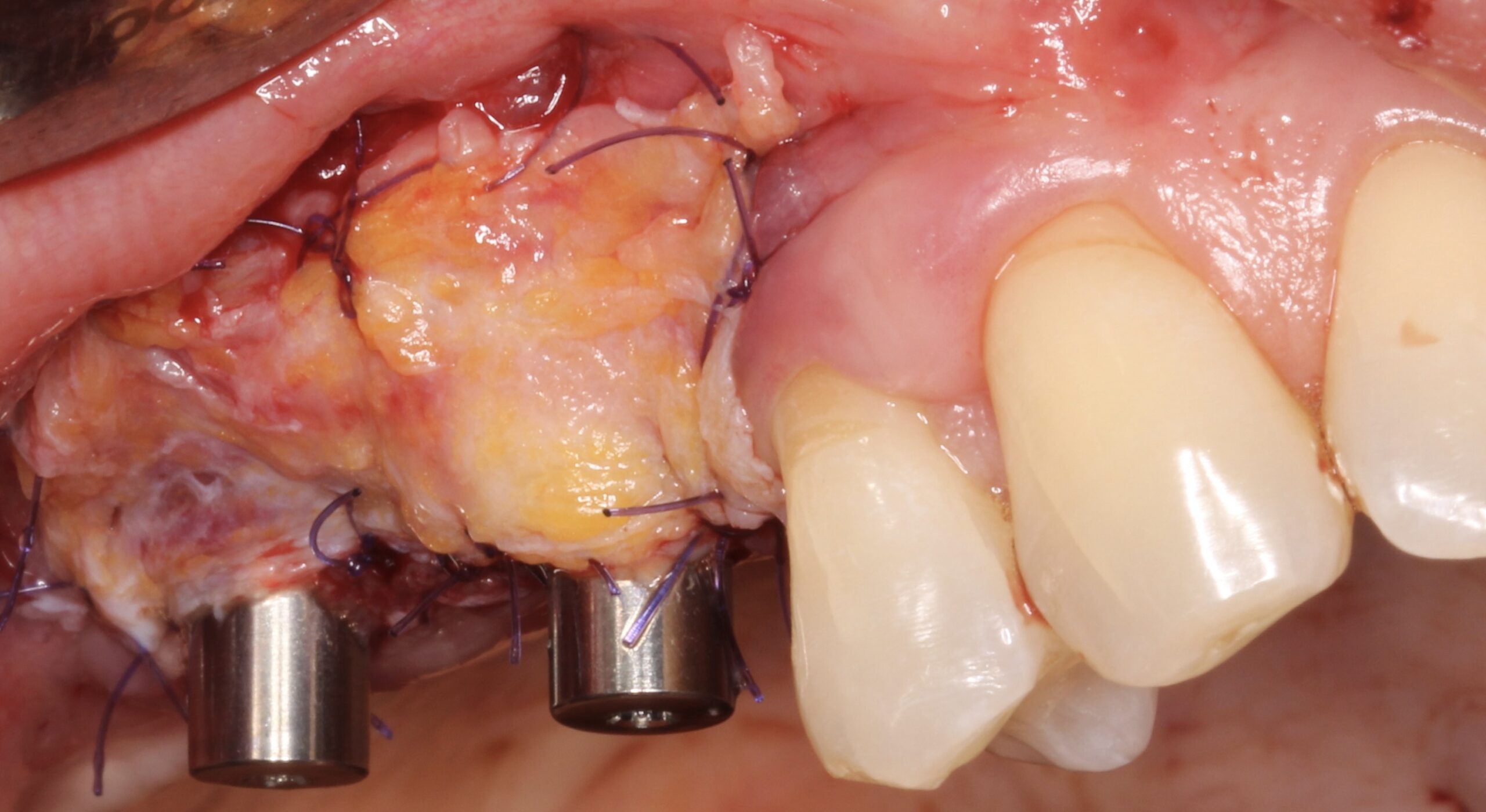
Figure 22.
2nd surgical phase was carried out and at the same time after raising a split-thickness flap the connective tissue graft was placed.

Figure 23.
1 year later clinical status of the implants and crowns was healthy.
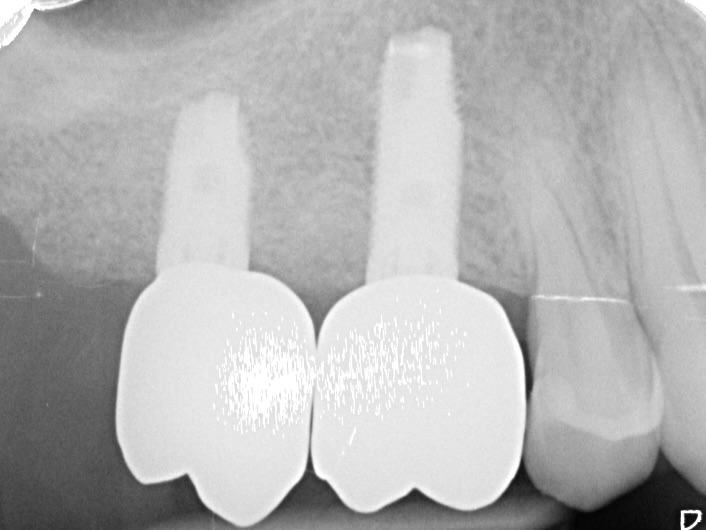
Figure 24.
1 year later radiographic status of the implants and crowns was healthy.
"Neoss ProActive® implant and NeoGen® non-resorbable, Ti-reinforced membrane is an excellent choice for the treatment of atrophic alveolar bone ridge on the aesthetic zone. The solution of bone dehiscences after implant placement by simultaneous GBR by using this protocol is fully predictable.
Dr. David González Spain 
